If you or someone you know has been diagnosed with epilepsy, you may be curious about the different medications available to treat this condition. In this article, we will take a closer look at anti-seizure drugs and provide an overview of the various options. Discover how these medications work to control seizures and what you can expect when starting epilepsy medication. Find out which factors may influence the choice of medication and the importance of working closely with your healthcare team to find the most suitable treatment for you or your loved one.
General Information about Epilepsy Medications
Understanding epilepsy
Epilepsy is a neurological disorder characterized by recurrent seizures. Seizures occur when there are sudden abnormal electrical or chemical discharges in the brain, leading to various symptoms such as loss of consciousness, convulsions, or abnormal movements. Epilepsy can affect people of all ages, and it is estimated that approximately 50 million people worldwide have this condition.
Purpose of anti-seizure drugs
The main goal of epilepsy medications, also known as anti-seizure or antiepileptic drugs, is to control or reduce the frequency and intensity of seizures. These medications work by stabilizing the electrical activity in the brain, preventing abnormal discharges that lead to seizures. It is important to note that epilepsy medications do not cure the underlying condition but help manage the symptoms.
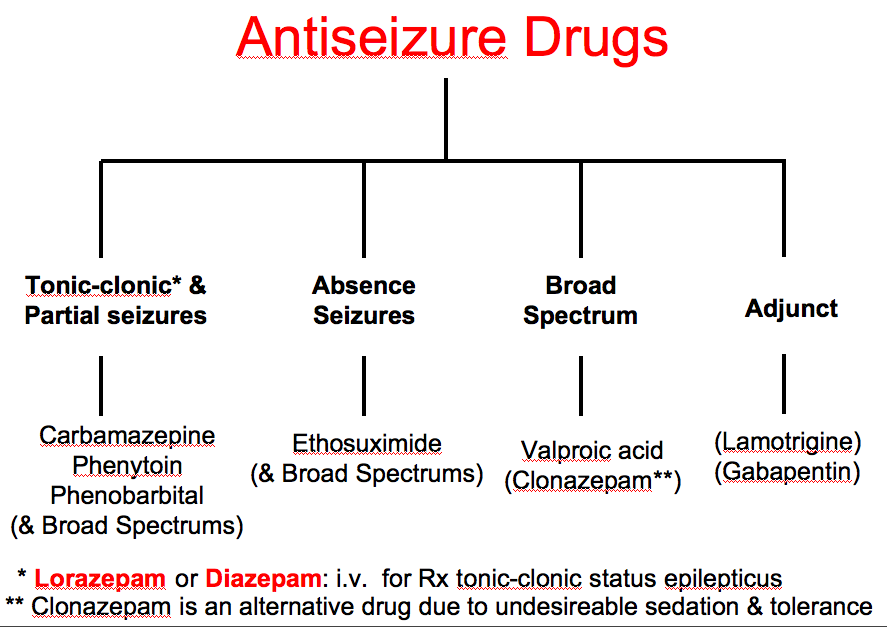
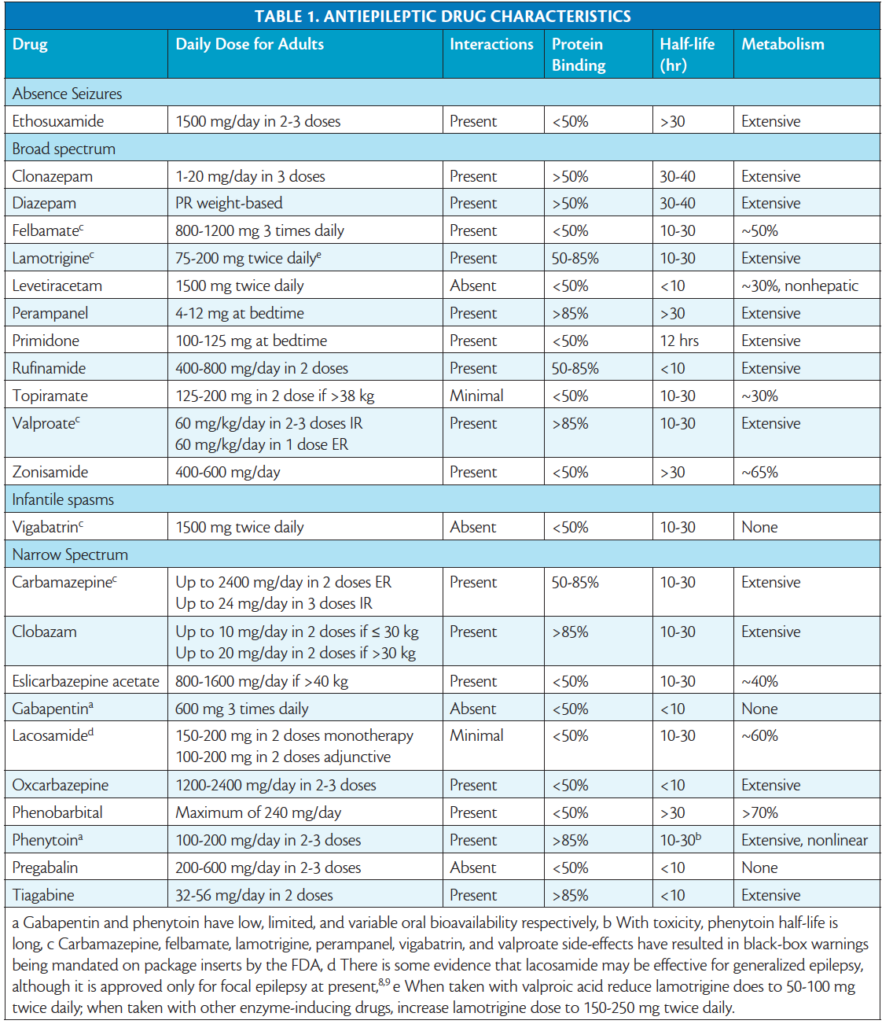
Overview of available medications
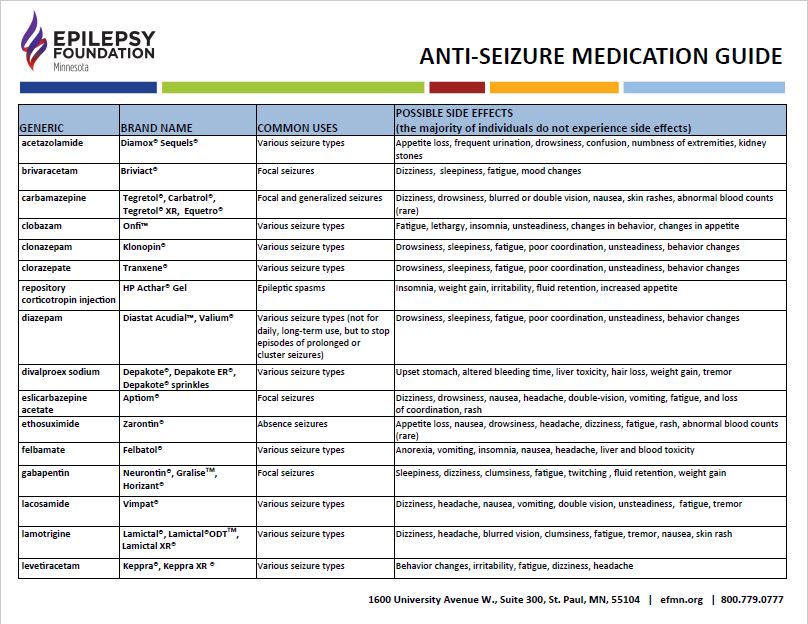
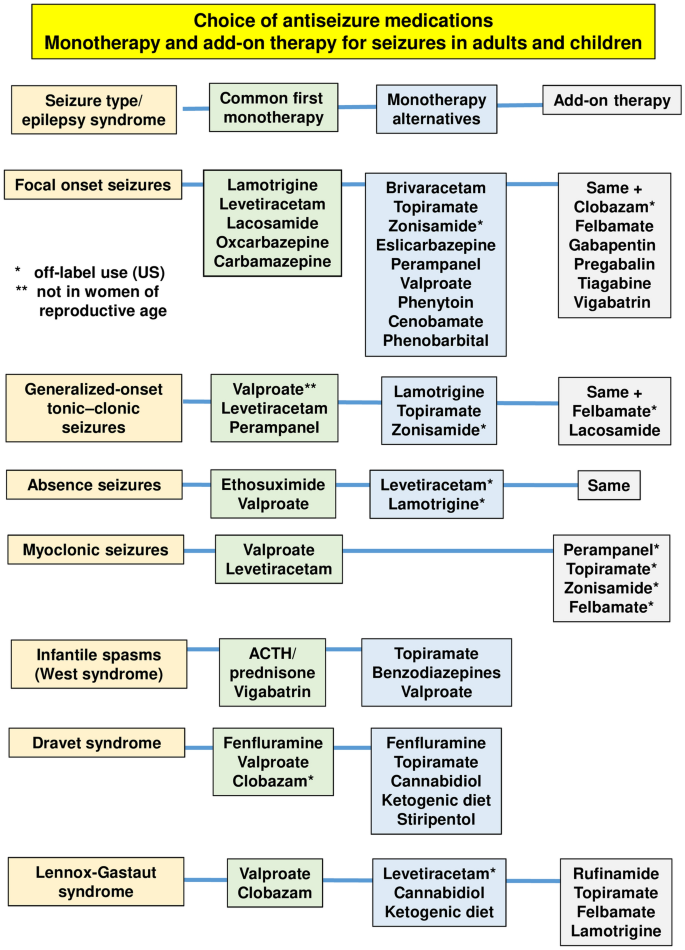
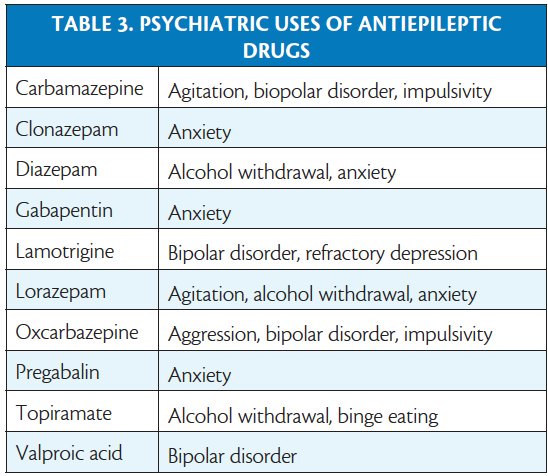
There is a wide range of anti-seizure medications available today, each with its own unique mechanism of action and potential side effects. These medications can be categorized into different classes based on their mode of action and are prescribed based on the type of seizures, the individual’s overall health, and other factors.
First-Line Anti-Seizure Medications
Carbamazepine
Carbamazepine is one of the most commonly prescribed medications for epilepsy. It belongs to the class of drugs known as sodium channel blockers and works by inhibiting the abnormal electrical activity in the brain. This medication is often used to treat focal seizures and tonic-clonic seizures. It is important to follow your doctor’s instructions carefully and be aware of potential side effects, such as dizziness, drowsiness, and skin rash.
Valproic acid
Valproic acid, also referred to as sodium valproate, is another commonly prescribed first-line medication for epilepsy. It works by increasing the levels of a neurotransmitter called gamma-aminobutyric acid (GABA) in the brain, which helps regulate electrical activity. Valproic acid is effective in treating a wide range of seizures, including absence seizures, focal seizures, and tonic-clonic seizures. However, it may cause side effects such as weight gain, hair loss, and liver problems, so regular monitoring is essential.
Lamotrigine
Lamotrigine, an anticonvulsant medication, is often used as a first-line treatment for partial seizures, absence seizures, and generalized tonic-clonic seizures. This medication inhibits the release of glutamate, a neurotransmitter that contributes to abnormal electrical activity in the brain. It is important to start lamotrigine at a low dose and gradually increase it to reduce the risk of serious skin reactions, a potential but rare side effect associated with this medication.
Second-Line Anti-Seizure Medications
Phenytoin
Phenytoin, a traditional anti-seizure medication, is primarily used for the treatment of focal seizures, tonic-clonic seizures, and status epilepticus. It works by stabilizing the electrical activity in the brain and reducing the occurrence of seizures. However, phenytoin has a narrow therapeutic range, which means that blood levels need to be carefully monitored to ensure effectiveness and prevent toxicity. Side effects may include dizziness, drowsiness, and enlarged gums.
Phenobarbital
Phenobarbital is a barbiturate medication commonly used as a second-line or adjunct treatment for seizures in both adults and children. It acts by enhancing the effects of GABA, thus reducing excitability in the brain. Despite its efficacy, phenobarbital may cause sedation and cognitive impairment, making it important to find the right balance between seizure control and quality of life.
Topiramate
Topiramate is a medication that is often prescribed as an adjunct therapy for focal seizures, tonic-clonic seizures, and Lennox-Gastaut syndrome. It is thought to work by blocking sodium channels and enhancing GABA activity. Topiramate may cause side effects such as drowsiness, difficulty concentrating, and an increased risk of kidney stones, so close monitoring and regular follow-ups with your doctor are crucial.
Newer Anti-Seizure Medications
Levetiracetam
Levetiracetam is a newer generation anti-seizure medication that is considered both safe and effective for a variety of seizure types. It works by inhibiting the release of neurotransmitters involved in seizure activity. Levetiracetam is commonly used to treat focal seizures, myoclonic seizures, and tonic-clonic seizures. Some individuals may experience side effects such as irritability, drowsiness, and headaches, but these are typically mild and temporary.
Oxcarbazepine
Oxcarbazepine is a newer medication that is structurally similar to carbamazepine but with a more favorable side effect profile. It is often prescribed for the treatment of focal seizures and can be used as a monotherapy or in combination with other anti-seizure medications. Common side effects include dizziness, drowsiness, and gastrointestinal disturbances, but these usually subside with time.
Eslicarbazepine acetate
Eslicarbazepine acetate is another newer medication that is closely related to oxcarbazepine. It is approved for the treatment of focal seizures and may be used as an add-on therapy when other medications are not providing adequate seizure control. Side effects may include dizziness, headache, and fatigue. It is important to note that eslicarbazepine acetate can interact with other medications, so it is essential to inform your healthcare provider about any other drugs you may be taking.
Combination Therapy
Rationale for combining medications
Combination therapy, also known as polytherapy, involves the use of two or more anti-seizure medications to achieve better seizure control. This approach is often considered when monotherapy fails to adequately control seizures or when the types of seizures require multiple mechanisms of action for effective management. The rationale behind combination therapy is to target different aspects of seizure activity and enhance overall seizure control.
Commonly used drug combinations
There are various combinations of anti-seizure medications that healthcare providers may prescribe based on individual needs. Some commonly used combinations include lamotrigine with valproic acid, carbamazepine with phenytoin, and levetiracetam with oxcarbazepine. It is crucial to work closely with your doctor to find the most effective combination while managing any potential side effects or drug interactions.
Non-Pharmacological Treatment Options
Ketogenic diet
The ketogenic diet is a high-fat, low-carbohydrate diet that has been shown to be effective in reducing seizures, particularly in children with epilepsy. The diet forces the body to enter a state of ketosis, where it primarily uses ketones (fat breakdown products) for energy instead of glucose. The exact mechanism of action is not fully understood, but it is believed that the diet alters brain metabolism and reduces seizure activity. The ketogenic diet requires careful monitoring and should only be implemented under the guidance of a healthcare professional.
Vagus nerve stimulation
Vagus nerve stimulation (VNS) is a non-pharmacological treatment option that involves the implantation of a device that delivers electrical impulses to the vagus nerve, which runs from the brain to various organs in the body. These electrical impulses help regulate abnormal brain activity and reduce the frequency and intensity of seizures. VNS therapy may be considered for individuals who do not respond well to medications or are not candidates for surgery. It is important to note that VNS requires continued monitoring and adjustments by a healthcare professional.
Neurosurgery
Neurosurgery may be an option for individuals with epilepsy who do not respond to medications or other treatments. Surgical interventions such as resective surgery, where the area of the brain responsible for seizures is removed, or neuromodulation techniques, where electrodes are implanted to deliver targeted electrical stimulation, can be effective in reducing or eliminating seizures. However, neurosurgery is a complex procedure and should only be considered after a comprehensive evaluation by a team of experienced healthcare professionals.
Side Effects and Risks
Common side effects
Epilepsy medications can cause various side effects, and the specific side effects depend on the individual, the medication, and the dosage. Common side effects may include drowsiness, dizziness, loss of coordination, nausea, and changes in mood or behavior. It is important to communicate any side effects experienced to your healthcare provider for appropriate management and adjustments to the treatment plan.
Serious risks and warnings
In addition to common side effects, some epilepsy medications may carry more serious risks and warnings. These can include an increased risk of suicidal thoughts or behavior, liver toxicity, bone density loss, and birth defects. It is crucial to closely follow your healthcare provider’s instructions, have regular check-ups, and promptly report any concerning symptoms. If you experience any severe or life-threatening reactions, seek medical attention immediately.
Managing Medication Dosages
Proper dosage adjustment
Finding the right dosage of epilepsy medications is essential for optimal seizure control and to minimize side effects. Dosages are typically started low and gradually increased until an effective level is reached. It is important to strictly follow your doctor’s instructions when taking medications, including adhering to the prescribed dosages, schedules, and any specific instructions regarding meals or interactions with other substances.
Blood tests and monitoring
Regular blood tests and monitoring are necessary when taking epilepsy medications to ensure therapeutic levels and evaluate any potential side effects or complications. Blood tests may be used to measure drug levels, monitor liver function, check for vitamin deficiencies, and assess other parameters. Compliance with scheduled tests and appointments is critical for effective management of epilepsy and medication adjustments, if needed.
Potential Drug Interactions
Effects of drug interactions
Epilepsy medications can interact with other drugs, including over-the-counter medications, herbal supplements, and even certain foods. Drug interactions can affect the effectiveness of medications or increase the risk of side effects. Some interactions may cause increased or decreased drug levels in the bloodstream or interfere with the metabolism of the medications. It is important to inform your healthcare provider about all the medications and substances you are using to minimize potential interactions.
Commonly interacting medications
Certain medications are known to significantly interact with epilepsy medications. Examples include birth control pills, certain antibiotics, anticoagulants, antidepressants, and antifungal drugs. Your healthcare provider should be informed about all the medications you are taking to ensure appropriate dosing and minimize any potential interactions. They may need to adjust your medication regimen or monitor your drug levels more closely.
Pregnancy and Epilepsy Medications
Managing epilepsy during pregnancy
Managing epilepsy during pregnancy requires special considerations to ensure the safety of both the mother and the developing baby. Some epileptic medications can potentially harm the fetus, while uncontrolled seizures can pose risks to both the mother and baby. It is essential for women with epilepsy who are considering becoming pregnant or are already pregnant to work closely with their healthcare provider to evaluate the risks and benefits of their current medication regimen and make any necessary adjustments.
Effects of medications on pregnancy
Some epilepsy medications have been associated with an increased risk of birth defects or other complications during pregnancy. However, every situation is unique, and the decision to continue or change medications should be based on a thorough evaluation of the risks and benefits. Healthcare providers may adjust the medication dosage, switch to a safer alternative, or monitor the pregnancy more closely to ensure the best possible outcome. It is crucial to have open and honest discussions with your healthcare provider and follow their recommendations during pregnancy.
In conclusion, epilepsy medications play a crucial role in managing seizures and improving the quality of life for individuals with epilepsy. There are various types of medications available, each with its own mechanisms of action and potential side effects. Depending on the specific needs and characteristics of the individual, different medications or combinations may be prescribed to achieve optimal seizure control. It is important to closely follow your healthcare provider’s instructions, communicate any side effects or concerns, and actively participate in the management of your epilepsy to ensure the most effective and safe treatment.