Living with rheumatoid arthritis can be challenging, but with the right nursing considerations and management, patients can find relief and improve their quality of life. In this article, we will explore the crucial nursing strategies and interventions that can help individuals with rheumatoid arthritis manage their symptoms effectively. From medication management to pain control techniques, we will discuss the various aspects of nursing care that play a vital role in supporting patients with this chronic condition. By implementing these considerations, nurses can empower individuals with rheumatoid arthritis to better manage their disease and lead fulfilling lives.
Assessment
Identifying the patient’s symptoms
As a nurse, one of your primary responsibilities is to assess and identify the patient’s symptoms when it comes to managing Rheumatoid Arthritis (RA). RA is a chronic autoimmune disease that primarily affects the joints and can cause severe pain, stiffness, and swelling. When assessing the patient, you should carefully listen and document their complaints of joint pain and any other symptoms they may be experiencing, such as fatigue or morning stiffness. It is important to ask about the duration and intensity of the pain, as well as any exacerbating or alleviating factors. This information will help in formulating an accurate nursing diagnosis and developing an appropriate care plan.
Performing a physical examination
A comprehensive physical examination is essential in the assessment of a patient with RA. During the examination, you should observe and palpate the joints for any signs of inflammation, tenderness, or deformity. It is particularly important to assess the small joints of the hands and feet, as they are often the earliest sites affected by RA. Range of motion should also be evaluated, noting any limitations or contractures. In addition to assessing the joints, you should also examine other systems of the body, as RA can have systemic manifestations. Pay close attention to the skin for any nodules or rashes, and listen to the heart and lungs to identify any potential cardiac or pulmonary complications.
Obtaining a medical history
Obtaining a thorough medical history is crucial in understanding the patient’s background and overall health. Inquiring about any prior diagnoses, surgeries, or medications can provide valuable insight into the patient’s medical background. It is important to ask about any previous treatments for RA, such as disease-modifying antirheumatic drugs (DMARDs) or corticosteroids, as this will affect the plan of care and medication management. Additionally, it is essential to assess the patient’s family history, as genetics can play a role in the development of RA. Taking the time to carefully gather this information will help in developing an individualized care plan for the patient.
Diagnosis
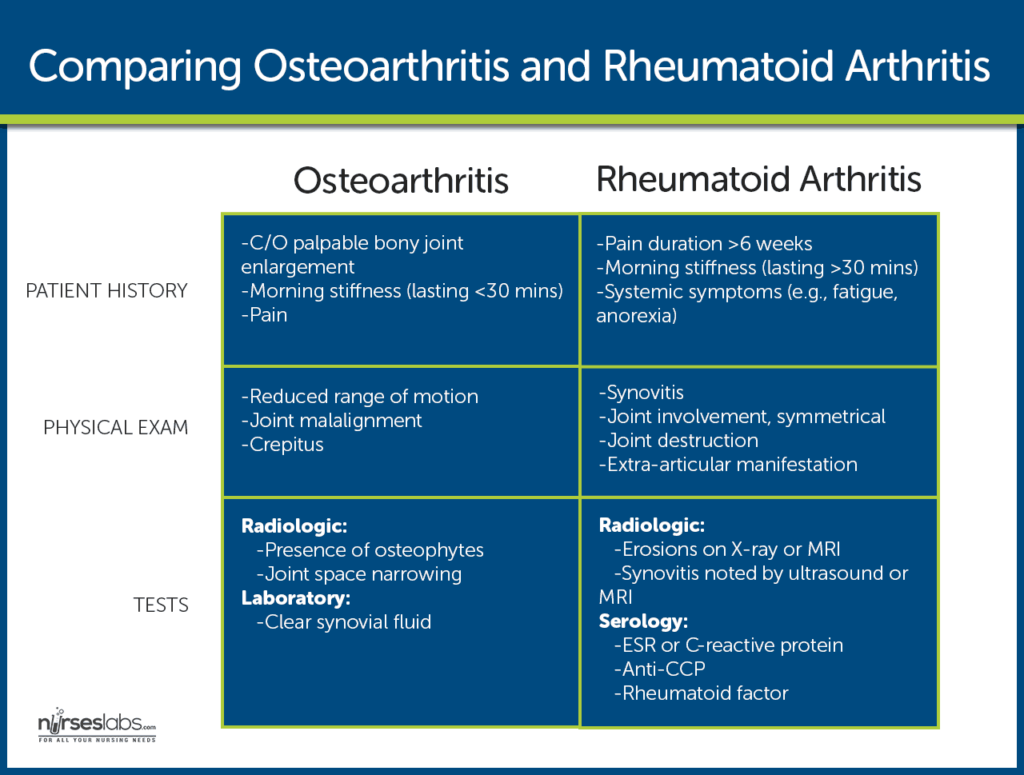
Laboratory tests and diagnostic procedures
Laboratory tests and diagnostic procedures are essential in diagnosing and monitoring the progression of RA. Blood tests such as rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) can help confirm the presence of RA and assess disease activity. Imaging studies, such as X-rays or magnetic resonance imaging (MRI), may also be performed to evaluate joint damage and deformities. These diagnostic tools, along with the patient’s clinical presentation, will help the healthcare team in formulating an accurate diagnosis.
Collaborating with other healthcare professionals
Collaboration with other healthcare professionals, particularly rheumatologists, physical therapists, and occupational therapists, is essential in managing RA. Rheumatologists specialize in the diagnosis and treatment of RA and will guide the overall management plan for the patient. Physical therapists and occupational therapists play a vital role in improving joint mobility and function through exercises and techniques. Collaborating with these professionals ensures a comprehensive and holistic approach to the patient’s care, addressing not only the medical aspects but also the rehabilitation needs.

Medication Management
Administering and monitoring the effectiveness of disease-modifying antirheumatic drugs (DMARDs)
Disease-modifying antirheumatic drugs (DMARDs) are the cornerstone of pharmacotherapy for RA. These medications help suppress the inflammatory process, slow down or halt the progression of the disease, and ultimately improve symptoms and prevent joint damage. As a nurse, you will play a key role in administering DMARDs to the patient, ensuring proper dosing and monitoring for any adverse effects. Regular assessments, such as blood tests, are essential to monitor the effectiveness and safety of these medications.
Administering nonsteroidal anti-inflammatory drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage the pain and inflammation associated with RA. These medications work by reducing inflammation and relieving pain, thereby improving the patient’s quality of life. As a nurse, you may be responsible for administering NSAIDs and monitoring for any adverse effects, such as gastrointestinal bleeding or kidney dysfunction. It is important to educate the patient on the proper use and potential side effects of NSAIDs.
Administering corticosteroids
Corticosteroids, such as prednisone, are powerful anti-inflammatory medications that can provide rapid relief of symptoms in patients with RA. However, these medications are typically used for short periods of time due to the potential for long-term side effects. As a nurse, you may be involved in administering corticosteroids and closely monitoring the patient for any adverse effects, such as hyperglycemia, osteoporosis, or immunosuppression. It is important to educate the patient on the short-term nature of corticosteroid therapy and the need for close monitoring.
Pain Management
Assessing and documenting the patient’s pain
Effective pain management is crucial for improving the patient’s quality of life in RA. As a nurse, you should assess and document the patient’s pain using appropriate pain assessment tools, such as a numeric rating scale or a visual analog scale. It is important to evaluate the location, intensity, and duration of the pain, as well as any factors that aggravate or alleviate it. Regular pain assessments will help in determining the effectiveness of pain management interventions and guide adjustments in the plan of care.
Collaborating with the healthcare team to develop a pain management plan
Collaboration with the healthcare team, including the patient and their family, is essential in developing an individualized pain management plan for the patient with RA. The team should work together to identify appropriate pharmacological and non-pharmacological interventions to effectively manage pain. Pharmacological interventions may include analgesics, such as acetaminophen or opioids, while non-pharmacological interventions may include heat or cold therapy, relaxation techniques, or transcutaneous electrical nerve stimulation (TENS). By collaborating and tailoring the pain management plan to the patient’s individual needs and preferences, optimal pain relief can be achieved.
Administering pain medication as prescribed
As a nurse, you will be responsible for administering pain medications to the patient as prescribed. It is important to carefully follow medication administration protocols, including the correct dose, route, and frequency. During medication administration, you should closely monitor the patient for any adverse effects or signs of inadequate pain relief. Open communication with the patient is key, as they may need to advocate for themselves if they are still experiencing pain or if the medication is causing significant side effects. Regular reassessment of the patient’s pain and adjustment of the pain management plan, if necessary, will help ensure optimal pain control.
Promotion of Joint Mobility
Educating the patient on joint protection techniques
Educating the patient on joint protection techniques is crucial in managing RA. As a nurse, you can play a significant role in teaching the patient how to minimize joint stress and reduce the risk of further damage. This may include providing guidance on proper body mechanics, such as using larger joints instead of smaller ones, and encouraging the use of assistive devices, such as canes or splints, to support and stabilize the joints. By promoting joint protection techniques, you can empower the patient to actively participate in their own care and prevent further joint deterioration.
Assisting the patient with range of motion exercises
Range of motion exercises are important in maintaining joint mobility and preventing contractures in patients with RA. You can assist the patient by demonstrating and guiding them through these exercises. It is important to encourage regular and gentle movements to reduce stiffness and improve joint function. Additionally, you should educate the patient on the importance of maintaining an appropriate balance between rest and activity to prevent excessive joint strain. Regular exercise can have a positive impact on the patient’s overall physical and mental well-being.
Collaborating with physical and occupational therapists
Collaboration with physical and occupational therapists is essential in promoting joint mobility for patients with RA. These professionals are experts in providing specialized exercises and techniques to improve joint function and address any limitations in activities of daily living. As a nurse, you can collaborate with physical and occupational therapists to ensure a coordinated and individualized plan of care for the patient. Together, you can work towards enhancing the patient’s independence and quality of life by optimizing joint mobility and function.
Nutritional Support
Assessing the patient’s nutritional status
Assessing the patient’s nutritional status is important in managing RA. As a nurse, you should evaluate the patient’s dietary intake and identify any deficiencies or excesses that may impact their overall health. It is essential to assess the patient’s weight, body mass index (BMI), and presence of any unintentional weight loss, as these can be indicators of malnutrition. Additionally, you should inquire about the patient’s dietary habits and preferences, as well as any food intolerances or allergies. By understanding the patient’s nutritional status, you can collaborate with a registered dietitian to develop a balanced diet plan tailored to their specific needs.
Collaborating with a registered dietitian to develop a balanced diet plan
Collaboration with a registered dietitian is crucial in developing a balanced diet plan for patients with RA. A dietitian specializes in assessing nutritional needs and can provide expert guidance on dietary modifications that may benefit the patient. For example, increasing the intake of omega-3 fatty acids found in fish or plant-based sources, such as flaxseeds or walnuts, may help reduce inflammation. Additionally, the dietitian can address any specific concerns, such as calcium and vitamin D intake for bone health or the impact of certain medications on nutrient absorption. Collaborating with a dietitian ensures that the patient receives comprehensive and individualized nutritional support.
Educating the patient on the importance of a healthy diet
Educating the patient on the importance of a healthy diet is essential in managing RA. As a nurse, you should take the opportunity to provide information and resources to the patient and their family on how dietary choices can impact their overall health and well-being. Emphasize the importance of consuming a variety of fruits, vegetables, whole grains, and lean proteins to provide essential nutrients and antioxidants. Encourage the patient to limit processed foods, sugary beverages, and foods high in saturated fats, as these can potentially exacerbate inflammation. By educating the patient on the role of nutrition in managing RA, you can empower them to make informed dietary choices that support their overall health.
Psychosocial Support
Assessing the patient’s emotional and psychological well-being
Assessing the patient’s emotional and psychological well-being is essential in providing holistic care for individuals with RA. As a nurse, you should establish a therapeutic relationship with the patient, creating a safe and supportive environment for them to express their concerns and emotions. Utilize assessment tools, such as the Patient Health Questionnaire (PHQ-9) or the Generalized Anxiety Disorder (GAD-7) scale, to screen for symptoms of depression or anxiety. Observe for any changes in the patient’s mood, behavior, or social interactions, as these may indicate underlying psychosocial challenges related to living with a chronic illness.
Providing emotional support and counseling
Providing emotional support and counseling is an important aspect of nursing care for patients with RA. As a nurse, you should be empathetic and attentive to the patient’s emotional needs, acknowledging the impact of living with a chronic condition on their overall well-being. Active listening and therapeutic communication techniques can help the patient feel heard and understood. Additionally, you can provide education and resources on coping strategies, stress management techniques, or relaxation exercises to promote emotional well-being. Referrals to support groups or mental health professionals may also be appropriate, depending on the patient’s needs and preferences.
Referring the patient to support groups or mental health professionals
Referring the patient to support groups or mental health professionals can greatly enhance the psychosocial support available to individuals with RA. Support groups provide an opportunity for patients to connect with others facing similar challenges, share experiences, and learn coping strategies. Mental health professionals, such as psychologists or counselors, have specialized training in addressing the emotional and psychological aspects of chronic illness. By referring the patient to these resources, you can ensure that they receive the appropriate level of support and care that extends beyond the medical management of their condition.
Management of Flare-Ups
Assessing the severity of the flare-up
Assessing the severity of a flare-up is essential in managing RA effectively. Flare-ups are characterized by the sudden worsening of symptoms, including increased joint pain, stiffness, and swelling. As a nurse, you should assess the patient’s pain intensity, joint tenderness, and functional limitations during a flare-up. Use appropriate pain assessment tools, such as the visual analog scale, to quantify the severity of the pain. This information will help guide adjustments in the patient’s medication or treatment plan to provide prompt relief and improve their overall comfort.
Collaborating with the healthcare team to adjust medication or treatment plan
Collaboration with the healthcare team is crucial during a flare-up to adjust the patient’s medication or treatment plan. As a nurse, you should communicate any changes in the patient’s symptoms or functional limitations to the healthcare team, particularly the rheumatologist. Based on this information, the team may recommend increasing the dosage of medications or adding additional therapies to manage the flare-up effectively. By collaborating and promptly adjusting the plan of care, the patient can experience relief from the acute exacerbation of symptoms and prevent long-term joint damage.
Providing comfort measures during the flare-up
Providing comfort measures during a flare-up is an important nursing consideration for patients with RA. As a nurse, you can offer non-pharmacological interventions to help alleviate pain and discomfort. Applying heat or cold therapy to affected joints, providing gentle massage, or assisting the patient with positioning to minimize additional stress on the joints can be effective strategies. Additionally, you should ensure that the patient receives adequate rest and sleep during a flare-up, as fatigue can exacerbate pain and impact overall well-being. By focusing on providing comfort and support during these challenging periods, you can contribute to the patient’s overall management and recovery.
Patient Education
Teaching the patient about the disease process and self-management strategies
Teaching the patient about the disease process and self-management strategies is a critical component of nursing care for patients with RA. As a nurse, you play a pivotal role in providing education and empowering the patient to actively participate in their own care. Take the time to explain the underlying pathophysiology of RA, including the immune system’s role and the potential long-term effects on joints and other body systems. Provide information on self-management strategies, such as joint protection techniques, exercise routines, and pain management strategies, to help the patient maintain their independence and optimize their quality of life.
Educating the patient on medication adherence and potential side effects
Educating the patient on medication adherence and potential side effects is essential in managing RA effectively. As a nurse, you should provide clear instructions on how and when to take prescribed medications, emphasizing the importance of adhering to the prescribed regimen. Educate the patient about the possible side effects of each medication and the appropriate course of action if side effects occur. Reinforce the importance of regular follow-up appointments and laboratory tests to monitor the effectiveness and safety of the medications. By promoting medication adherence and providing education on potential side effects, you can enhance the patient’s overall disease management.
Providing resources for further education and support
Providing resources for further education and support is crucial in empowering the patient to actively manage their RA. As a nurse, you should be knowledgeable about reliable sources of information, such as reputable websites, patient education materials, or community resources. Share these resources with the patient and their family, encouraging them to explore further and ask questions. Additionally, inform the patient about available support groups or advocacy organizations that can provide additional education and emotional support. By equipping the patient with valuable resources, you contribute to their ongoing education and overall well-being.
Collaboration with Other Healthcare Professionals
Communicating with rheumatologists, physical therapists, and occupational therapists
Communicating with rheumatologists, physical therapists, and occupational therapists is vital in providing comprehensive care for patients with RA. As a nurse, you serve as a crucial link between these healthcare professionals and the patient. Regularly share pertinent patient information, such as changes in symptoms, treatment response, or functional limitations, with the healthcare team. This open line of communication ensures that the patient’s care is coordinated, individualized, and consistent across all disciplines. By facilitating effective communication, you contribute to the overall success of the patient’s management plan.
Participating in interdisciplinary care meetings
Participating in interdisciplinary care meetings is essential in ensuring a holistic and coordinated approach to the patient’s care. These meetings bring together healthcare professionals from various disciplines, such as rheumatology, nursing, physical therapy, and occupational therapy, to discuss the patient’s progress, address any challenges, and adjust the plan of care as needed. As a nurse, your input during these meetings is valuable, as you provide firsthand observations and insights into the patient’s condition and response to interventions. By actively participating in interdisciplinary care meetings, you contribute to the collaborative nature of the patient’s care and facilitate optimal outcomes.
Coordinating care and referrals for specialized services
Coordinating care and referrals for specialized services is an important aspect of nursing management for patients with RA. As a nurse, you should ensure that all necessary healthcare services and referrals are arranged and implemented efficiently. For example, if the patient requires specialized imaging, physical therapy, or counseling services, you should coordinate the necessary appointments and provide the patient with the required information. Follow up on referrals to ensure that the patient receives timely and appropriate care. By coordinating the patient’s care and facilitating access to specialized services, you contribute to their overall management and well-being.

