You’re about to embark on a journey of understanding bronchiectasis, a respiratory condition that affects the airways in your lungs. This article will provide you with a comprehensive overview of the causes, symptoms, and treatments associated with bronchiectasis. Whether you’re seeking information for yourself or looking to support a loved one, this article will equip you with the knowledge needed to navigate this condition with confidence and clarity. So, let’s delve into the realm of bronchiectasis and discover how it can impact your life.
Understanding Bronchiectasis: Causes, Symptoms, and Treatments
Bronchiectasis is a chronic lung condition that affects the bronchial tubes, which are the airways that carry air in and out of the lungs. In this comprehensive article, we will delve into the causes, symptoms, and various treatment options available for bronchiectasis. By understanding this condition better, you can take the necessary steps to manage it effectively and improve your quality of life.
Overview of Bronchiectasis
Definition and Description
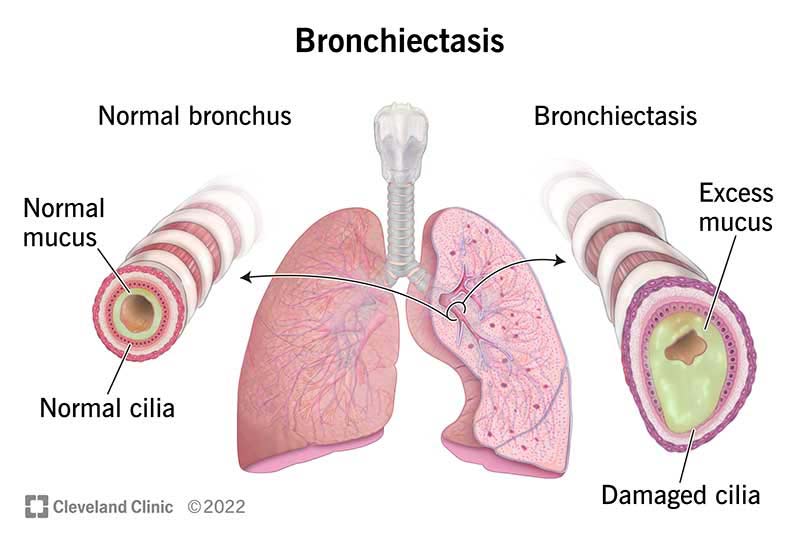
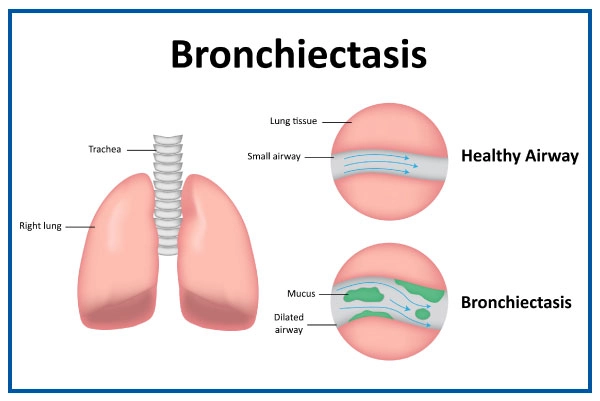
Bronchiectasis is characterized by permanent widening and scarring of the bronchial tubes. This condition impairs the normal clearance of mucus from the lungs, leading to the accumulation of mucus and bacteria. Over time, this can result in recurrent lung infections and progressive lung damage.
History and Prevalence
Bronchiectasis has been recognized for centuries, with descriptions dating back as far as ancient Egypt. However, advancements in medical diagnostics and treatments have improved the understanding and management of this condition. The prevalence of bronchiectasis varies worldwide, with some reports suggesting that it affects approximately 1 in 1000 individuals.
Anatomy of the Lungs
To better understand bronchiectasis, it is essential to familiarize yourself with the anatomy of the lungs. The lungs are made up of a complex system of airways, including the trachea, bronchi, and bronchioles. The bronchial tubes, or bronchi, branch off from the trachea and extend into the lungs, where they further divide into smaller airways called bronchioles. These airways are lined with a layer of cells that produce mucus, which helps trap foreign particles and clears them out through the action of tiny hair-like structures called cilia.
How Bronchiectasis Affects the Lungs
In bronchiectasis, the normal clearance mechanism of mucus is impaired. This leads to the buildup of mucus, bacteria, and other irritants in the bronchial tubes. The ongoing inflammation and infection contribute to the widening and scarring of the airways. As a result, the bronchial tubes become less efficient in delivering air to the lungs, leading to symptoms and complications associated with bronchiectasis.
Causes of Bronchiectasis
Infections
One of the primary causes of bronchiectasis is recurrent or chronic lung infections. Infections that can lead to bronchiectasis include pneumonia, tuberculosis, whooping cough, and non-tuberculous mycobacterial infections. These infections damage the airways and impair the normal clearance of mucus, leading to the development of bronchiectasis.
Genetic Causes
Some individuals may develop bronchiectasis due to genetic factors. Conditions such as cystic fibrosis, primary ciliary dyskinesia, alpha-1 antitrypsin deficiency, and immunodeficiency disorders can increase the risk of developing bronchiectasis. These genetic abnormalities affect the structure and function of the airways, making individuals more susceptible to recurrent infections and bronchiectasis.
Obstruction
The obstruction of the airways can also lead to the development of bronchiectasis. This can occur due to inhaled objects, lung tumors, or mucus plugs. When the airways are partially or completely blocked, the accumulation of mucus and bacteria occurs, leading to inflammation and scarring.
Autoimmune Disorders
Certain autoimmune disorders, such as rheumatoid arthritis and Sjogren’s syndrome, can contribute to the development of bronchiectasis. These conditions cause inflammation and damage to the airways, leading to bronchiectasis.
Risk Factors for Developing Bronchiectasis
Age
Bronchiectasis can affect individuals of any age, but it is more commonly diagnosed in middle-aged and older adults. As we age, the natural defense mechanisms of the lungs may weaken, making us more susceptible to infections and lung damage.
Prolonged Lung Infections
Recurrent or chronic lung infections, particularly if left untreated or inadequately managed, can significantly increase the risk of developing bronchiectasis. It is vital to seek treatment for lung infections promptly and adequately follow prescribed treatment plans to reduce the risk of complications.
Cystic Fibrosis
Cystic fibrosis is a genetic disorder characterized by the production of thick, sticky mucus that clogs the airways and other organs. Individuals with cystic fibrosis have a higher risk of developing bronchiectasis due to the chronic lung infections and impaired mucus clearance associated with the condition.
Immunodeficiency Disorders
Immune system disorders, such as HIV/AIDS or common variable immunodeficiency, weaken the body’s ability to fight off infections. This can increase the risk of recurrent lung infections and subsequently lead to the development of bronchiectasis.
Smoking
Smoking is a significant risk factor for developing bronchiectasis. The harmful chemicals in tobacco smoke can damage the airways, impairing their ability to clear mucus and increasing the risk of lung infections. Quitting smoking is crucial in preventing the development or progression of bronchiectasis.
Other Lung Conditions
Having other pre-existing lung conditions, such as chronic obstructive pulmonary disease (COPD), asthma, or bronchitis, can increase the risk of developing bronchiectasis. These conditions cause ongoing inflammation and damage to the airways, making individuals more susceptible to bronchiectasis.

Signs and Symptoms of Bronchiectasis
Chronic Cough
A persistent cough that lasts for months, with or without the production of mucus, is a common symptom of bronchiectasis. The cough is often worse in the morning or after physical activity.
Production of Excessive Sputum
People with bronchiectasis often produce large amounts of thick, sticky mucus or sputum. This can be difficult to clear from the lungs, leading to a sensation of congestion and frequent throat clearing.
Shortness of Breath
As bronchiectasis progresses, the airways become increasingly damaged, making it harder for air to flow in and out of the lungs. This can result in shortness of breath, particularly during physical exertion or when lying flat.
Chest Pain
Chest pain is a symptom that can occur in individuals with bronchiectasis. This pain is often described as a dull, aching sensation and may be exacerbated by coughing or deep breathing.
Fatigue and Weakness
The ongoing inflammation and recurrent lung infections associated with bronchiectasis can lead to fatigue and general feelings of weakness. This can impact daily activities and overall quality of life.
Recurrent Chest Infections
Frequent bouts of chest infections, such as pneumonia or bronchitis, are common in individuals with bronchiectasis. These infections may present with symptoms such as fever, increased cough, and worsening shortness of breath.
Diagnosing Bronchiectasis
Medical History and Physical Examination
If bronchiectasis is suspected, your healthcare provider will start by taking a detailed medical history and performing a physical examination. They will ask about your symptoms, medical conditions, and any possible risk factors for bronchiectasis.
Chest X-rays and Other Imaging Tests
Imaging tests, such as chest X-rays, computed tomography (CT) scans, or high-resolution CT scans, are commonly used to visualize the structure of the lungs. These tests can help identify thickened and dilated bronchial tubes, which are characteristic of bronchiectasis.
Sputum Culture
A sputum culture may be done to identify any bacterial or fungal infections that may be contributing to your symptoms. Taking a sample of your sputum and sending it to a laboratory for analysis helps determine if a specific type of bacteria or fungus is causing the lung infections.
Bronchoscopy
Bronchoscopy is an invasive procedure that allows the healthcare provider to visualize the airways directly. A thin tube with a camera at the end is inserted through the nose or mouth into the lungs. This procedure may be done to assess the extent of the bronchiectasis and rule out other underlying conditions.
Pulmonary Function Testing
Pulmonary function tests measure how well your lungs are functioning and can help assess the severity of bronchiectasis. These tests involve breathing into a machine that measures various lung volumes and capacities.
Complications Associated with Bronchiectasis
Lung Infections
Bronchiectasis increases the risk of recurrent lung infections, including pneumonia, bronchitis, and mycobacterial infections. These infections can be severe and lead to further lung damage, respiratory failure, or even sepsis if left untreated.
Respiratory Failure
In advanced stages of bronchiectasis, the lungs may become so damaged that they can no longer effectively oxygenate the blood or remove carbon dioxide. This can lead to respiratory failure, which requires immediate medical intervention.
Hemoptysis
Hemoptysis refers to coughing up blood from the respiratory tract. Individuals with bronchiectasis have an increased risk of experiencing hemoptysis due to the fragile blood vessels in the damaged airways.
Pneumonia
Recurrent lung infections in individuals with bronchiectasis can lead to pneumonia. This is a serious infection that can cause further lung damage and may require hospitalization and intensive treatment.
Cor Pulmonale
Cor pulmonale is a condition that occurs when the right side of the heart becomes enlarged and weakened due to lung disease. In bronchiectasis, chronic inflammation and lung damage can contribute to the development of cor pulmonale.
Treating Bronchiectasis
Goal of Treatment
The goal of treating bronchiectasis is to manage symptoms, prevent complications, and slow down the progression of lung damage. An individualized treatment plan will be developed based on the severity of the condition and individual needs.
Antibiotics
Antibiotics are often prescribed to treat and prevent lung infections in individuals with bronchiectasis. The choice of antibiotic will depend on the specific bacteria or fungal species identified in sputum cultures.
Mucus-Thinning Medications
Mucus-thinning medications, such as mucolytics, can help make the mucus in the airways thinner and easier to clear from the lungs. These medications can improve symptoms and reduce the risk of recurrent lung infections.
Bronchodilators
Bronchodilators, such as inhalers or nebulizers, may be prescribed to help open up the airways and make breathing easier. These medications can provide symptom relief and improve lung function.
Chest Physiotherapy
Chest physiotherapy techniques, such as postural drainage and percussion, can help loosen and remove mucus from the lungs. These techniques are often taught by respiratory therapists and can be performed at home or in a healthcare setting.
Pulmonary Rehabilitation
Pulmonary rehabilitation programs can help individuals with bronchiectasis improve their lung function, manage symptoms, and enhance their overall physical conditioning. These programs may include exercise training, breathing exercises, education on managing the condition, and support from healthcare professionals.

Medical Treatments for Bronchiectasis
Pulmonary Rehabilitation
Pulmonary rehabilitation programs can play a crucial role in managing bronchiectasis. These programs are typically conducted in a supervised setting and may include exercises to improve lung function, breathing techniques, and education on self-management.
Oxygen Therapy
In more severe cases of bronchiectasis, supplemental oxygen therapy may be required. This involves breathing in oxygen through a mask or nasal prongs to ensure that your body receives adequate amounts of oxygen.
Lung Transplantation
For individuals with end-stage bronchiectasis and significant lung damage, lung transplantation may be an option. This procedure involves replacing the diseased lungs with healthy donor lungs. Lung transplantation is a complex and costly procedure that requires careful evaluation and consideration.
Experimental Therapies
Various experimental therapies and treatments are being studied for the management of bronchiectasis. These may include new medications, gene therapy, or regenerative therapies. It is essential to discuss with your healthcare provider if you are interested in participating in clinical trials or exploring these experimental treatments.
Lifestyle Changes and Self-Care for Bronchiectasis
Quitting Smoking
If you are a smoker, quitting smoking is vital in managing bronchiectasis. Smoking further damages the airways and increases the risk of recurrent lung infections. Your healthcare provider can provide resources and support to help you quit smoking.
Managing Stress
Stress can worsen symptoms and affect your overall well-being. Finding effective stress management techniques, such as deep breathing exercises, meditation, or engaging in hobbies, can help reduce the impact of stress on your condition.
Eating a Healthy Diet
A healthy diet can support your overall health and immune function. Including a variety of fruits, vegetables, lean proteins, and whole grains in your diet can provide essential nutrients to support your body’s ability to fight off infections and manage inflammation.
Staying Active and Exercising
Regular exercise can help improve your lung function, strengthen your respiratory muscles, and enhance your overall endurance. Work with your healthcare provider to develop an exercise plan that suits your abilities and health condition.
Avoiding Lung Irritants
Reducing exposure to lung irritants, such as secondhand smoke, air pollution, and chemical fumes, is essential in managing bronchiectasis. If you have workplace exposures, discuss with your employer to find ways to minimize your risk.
Vaccinations
Ensuring you are up to date on vaccinations, such as the flu vaccine and pneumonia vaccine, is crucial in preventing respiratory infections that can worsen bronchiectasis. Talk to your healthcare provider about recommended vaccinations for your specific situation.
In conclusion, bronchiectasis is a chronic lung condition that requires ongoing management to control symptoms and prevent complications. By understanding the causes, symptoms, and treatment options available, you can work collaboratively with your healthcare provider to develop an individualized plan for managing bronchiectasis effectively. Remember, early diagnosis and proactive management are key in optimizing your lung health and overall well-being.