Imagine waking up one day with a pounding headache, fever, and a stiff neck that makes even the simplest movements excruciatingly painful. Your mind races with worry, not knowing what could be causing these distressing symptoms. In this article, we will shed light on the perplexing disease known as meningitis, exploring its causes, symptoms, and the available treatment options. Prepare to gain a deeper understanding of this condition, empowering you to recognize the signs and take action, should the need arise.
Causes of Meningitis
Meningitis is an infection that causes inflammation of the meninges, the protective membranes that surround the brain and spinal cord. There are several different causes of meningitis, including bacterial, viral, and fungal infections. Each type of meningitis has distinct characteristics and requires different treatment approaches.
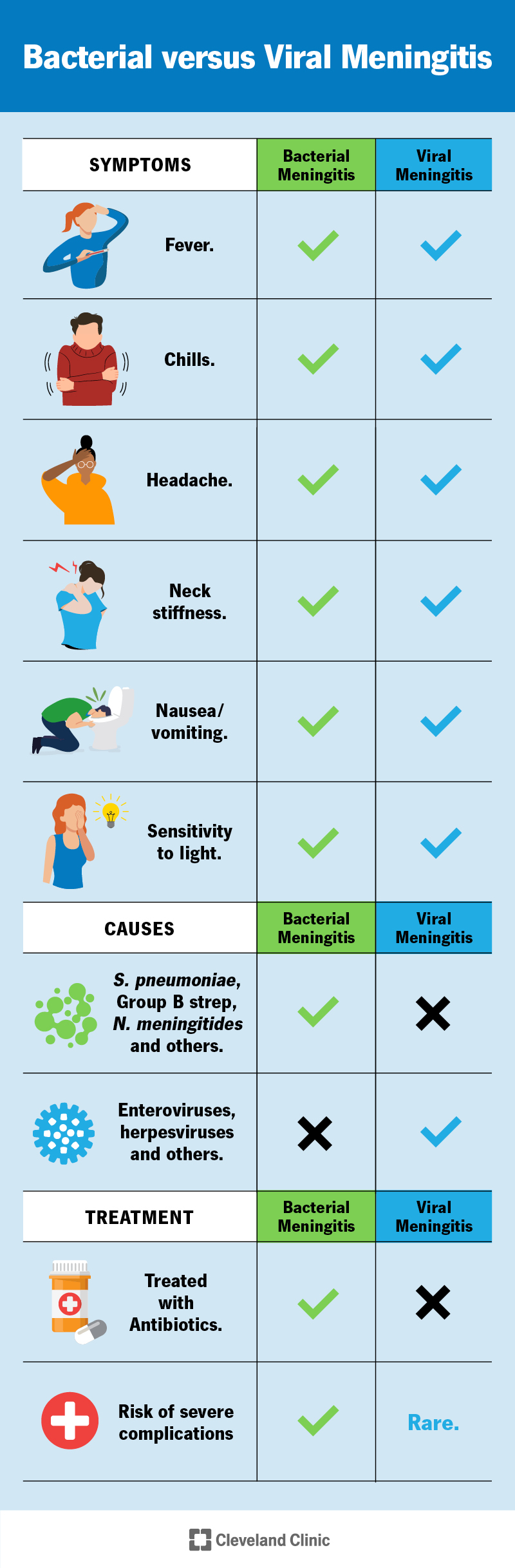
Bacterial Meningitis
Bacterial meningitis is caused by certain bacteria that can enter the bloodstream and travel to the brain and spinal cord. The most common bacteria that cause meningitis include Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Bacterial meningitis is a serious and potentially life-threatening condition that requires immediate medical attention.
Viral Meningitis
Viral meningitis, also known as aseptic meningitis, is caused by a viral infection. The most common viruses that cause viral meningitis are enteroviruses, such as Coxsackievirus and echovirus. Unlike bacterial meningitis, viral meningitis is usually less severe and resolves on its own without specific treatment. However, it is still important to seek medical evaluation and treatment to manage symptoms and prevent complications.
Fungal Meningitis
Fungal meningitis is a rare form of meningitis caused by certain types of fungi. This type of meningitis often occurs in individuals with weakened immune systems, such as those with HIV/AIDS or undergoing cancer treatment. Fungal meningitis can be a chronic and challenging condition to treat, requiring long-term antifungal medication and close medical monitoring.
Risk Factors
Certain factors can increase your risk of developing meningitis. It is important to be aware of these risk factors and take preventive measures to reduce your chances of infection.
Age
Meningitis can affect individuals of all ages, but certain age groups are more susceptible to specific types of meningitis. For example, bacterial meningitis is more common in infants and young children, while viral meningitis is more common in adolescents and young adults. Older adults and individuals with weakened immune systems are also at higher risk for developing meningitis.
Weakened Immune System
Having a weakened immune system can make you more vulnerable to infections, including meningitis. Conditions that can weaken the immune system include HIV/AIDS, certain types of cancer, organ transplantation, and long-term use of immunosuppressive medications. It is important to work with your healthcare provider to manage any underlying medical conditions and take necessary precautions to protect your health.
Close Contact with Infected Individuals
Meningitis is often spread through respiratory droplets from an infected person. Close contact with someone who has meningitis, such as living in the same household or attending crowded gatherings, increases the risk of transmission. It is important to practice good hygiene and avoid close contact with individuals who are sick or have been diagnosed with meningitis.
Living in Crowded Environments
Living in crowded environments, such as dormitories, military barracks, or correctional facilities, can increase the risk of meningitis transmission. The close proximity and shared living spaces in these settings can facilitate the spread of bacteria and viruses. Taking preventive measures, such as practicing good hygiene and getting vaccinated, can help reduce the risk of meningitis in these environments.
Traveling to Endemic Areas
Certain geographic regions have a higher prevalence of meningitis, known as meningitis-endemic areas. Traveling to these areas, particularly in sub-Saharan Africa during the dry season, can increase the risk of meningitis. It is important to be aware of the specific risks associated with your travel destination and take appropriate preventive measures, such as vaccination and practicing good hygiene.

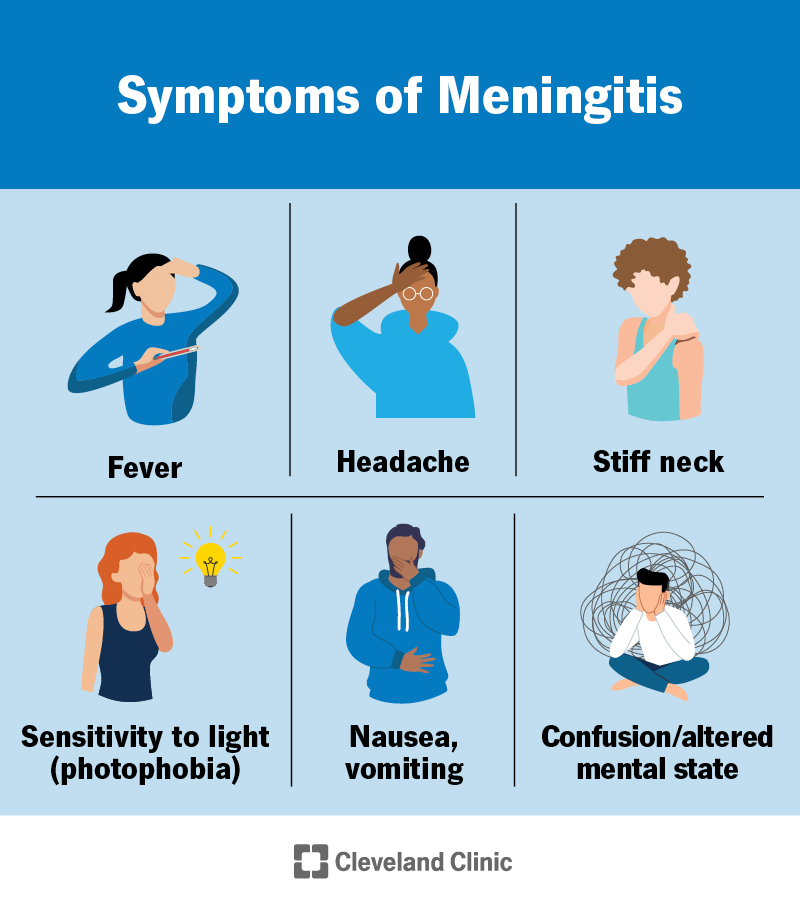
Signs and Symptoms
Recognizing the signs and symptoms of meningitis is crucial for early detection and prompt medical intervention. The symptoms of meningitis can vary depending on the cause and the individual, but there are several common symptoms to be aware of.
Fever and Headache
Fever and headache are often the initial symptoms of meningitis. The sudden onset of high fever, accompanied by severe headache, can be a sign of an infection affecting the central nervous system. The fever may persist and be resistant to over-the-counter fever-reducing medications.
Stiff Neck
A stiff neck is another hallmark symptom of meningitis. If you experience difficulty moving your neck forward or sideways, or if you experience neck pain or stiffness, it could be a sign of meningitis. Neck stiffness is caused by inflammation in the meninges, which limits the range of motion in the neck.
Nausea and Vomiting
Nausea and vomiting are common symptoms of meningitis, often accompanying the headache and fever. These symptoms can contribute to dehydration and electrolyte imbalances, so it is important to stay hydrated and seek medical attention if they persist.
Sensitivity to Light
Meningitis can also cause sensitivity to light, known as photophobia. Bright lights, sunlight, or even normal indoor lighting may be uncomfortable and painful to your eyes. This sensitivity is a result of the inflammation in the meninges, which can irritate the nerves responsible for processing light.
Changes in Mental Status
Meningitis can affect mental function and lead to changes in mental status. Confusion, irritability, difficulty concentrating, and even altered consciousness or coma can occur in severe cases of meningitis. These changes in mental status are due to the inflammation affecting the brain and can be a medical emergency requiring immediate attention.
Rash (in certain cases)
In some cases of bacterial meningitis, a characteristic rash may develop. This rash is known as petechiae and consists of small, purple or red spots on the skin that do not fade when pressed. The rash is caused by bleeding under the skin and can be an indication of a serious bacterial infection.
Seizures (in severe cases)
In severe cases of meningitis, seizures may occur. Seizures are caused by abnormal electrical activity in the brain and can manifest as convulsions or uncontrollable movements. If you or someone you know experiences a seizure, it is important to seek immediate medical attention.
Diagnostic Procedures
To confirm a diagnosis of meningitis, healthcare professionals will conduct several diagnostic procedures. These procedures help identify the cause of meningitis and determine the appropriate treatment plan.
Physical Examination
During the physical examination, your healthcare provider will assess your symptoms, including fever, headache, neck stiffness, and any accompanying neurological signs. They will also check for the presence of a rash, as well as evaluate your mental status and overall physical condition.
Lumbar Puncture
A lumbar puncture, also known as a spinal tap, is a procedure in which a small amount of cerebrospinal fluid (CSF) is removed from your spine using a thin needle. The CSF is then analyzed in a laboratory to determine if there are any abnormalities, such as the presence of bacteria, viruses, or fungi. A lumbar puncture is a key diagnostic procedure for meningitis.
Blood Tests
Blood tests may be performed to check for signs of infection, inflammation, or other abnormalities in the body. These tests can provide important information about the cause and severity of meningitis.
Imaging Studies
In some cases, imaging studies such as a CT scan or MRI may be ordered to evaluate the brain and spinal cord for any abnormalities, such as swelling or abscesses. These imaging studies can help guide further treatment decisions and provide a more comprehensive evaluation of the central nervous system.

Treatment Options
The treatment of meningitis depends on the cause of the infection. Prompt medical intervention is essential to prevent complications and improve outcomes. Treatment options for meningitis include:
Antibiotics (for Bacterial Meningitis)
Bacterial meningitis is treated with antibiotics to eliminate the bacterial infection. The choice of antibiotics depends on the specific bacteria causing the meningitis and may require intravenous administration. It is important to start antibiotics as soon as possible to prevent the spread of the infection and reduce the risk of complications.
Antiviral Medications (for Viral Meningitis)
Viral meningitis is typically managed with supportive care, as most cases resolve on their own without specific antiviral medications. However, if the cause of viral meningitis is known and can be treated with antiviral medications, such as herpes viral meningitis, specific antiviral drugs may be prescribed.
Antifungal Medications (for Fungal Meningitis)
Fungal meningitis requires long-term treatment with antifungal medications. These medications may need to be administered intravenously and for an extended period of time. Close monitoring and follow-up with a healthcare provider are necessary to ensure the effectiveness of the antifungal treatment.
Supportive Care
Supportive care plays a crucial role in the management of meningitis. This may include measures such as bed rest, fluid and electrolyte replacement, and pain relief. Supportive care aims to alleviate symptoms, provide comfort, and promote recovery.
Intravenous Fluids
Intravenous fluids may be administered to ensure hydration and maintain electrolyte balance. Dehydration is a common complication of meningitis due to fever, vomiting, and a decreased desire to drink fluids. Replenishing fluids intravenously can help prevent dehydration and support the body’s healing process.
Pain Relief
Pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to alleviate symptoms of headache, body aches, and general discomfort. It is important to follow the healthcare provider’s instructions and not exceed the recommended dosage.
Fever Management
Fever management is an important aspect of meningitis treatment. High fevers can be uncomfortable and potentially harmful, especially in children. Fever-reducing medications, such as acetaminophen or ibuprofen, may be recommended to help bring down the temperature and provide relief.
Hospitalization (in severe cases)
Severe cases of meningitis, particularly bacterial meningitis, may require hospitalization for close monitoring and intensive medical care. Hospitalization allows for continuous evaluation of the patient’s condition and administration of necessary treatments, such as intravenous antibiotics or antifungal medications.
Prevention and Vaccination
Prevention is key in reducing the risk of meningitis. Vaccination and good hygiene practices can help protect against meningitis and prevent its spread.
Vaccination for Bacterial Meningitis
Vaccination is available for certain types of bacterial meningitis. The vaccines are typically administered during childhood and adolescence, and may require booster doses in adulthood. The vaccines protect against the common bacteria that cause meningitis, such as Streptococcus pneumoniae and Neisseria meningitidis.
Vaccination for Viral Meningitis
Currently, there is no specific vaccine available to prevent viral meningitis caused by enteroviruses. However, routine childhood vaccinations, such as those against measles, mumps, rubella, and varicella (chickenpox), can help prevent certain viral infections that can lead to meningitis.
Practice Good Hygiene
Practicing good hygiene is essential in preventing the spread of meningitis. This includes frequently washing your hands with soap and water, covering your mouth and nose when coughing or sneezing, and avoiding sharing personal items, such as utensils or drinking glasses. These simple measures can significantly reduce the risk of infection.
Avoiding Close Contact with Infected Individuals
When someone in your household or close social circle is diagnosed with meningitis, it is important to take precautions to avoid close contact with the infected individual. This includes minimizing physical contact, such as hugging or kissing, and avoiding sharing personal items. If you develop symptoms, seek medical attention promptly.
Maintaining a Healthy Immune System
A strong immune system is essential in defending against infections, including meningitis. To maintain a healthy immune system, it is important to adopt a balanced lifestyle that includes regular exercise, a nutritious diet, adequate sleep, stress management, and avoiding smoking or excessive alcohol consumption. These measures can bolster your immune system and reduce the risk of infections.

Complications
Meningitis can lead to various complications, especially if not promptly diagnosed and treated. Common complications include:
Hearing Loss
Meningitis can cause permanent hearing loss in some cases. The inflammation in the meninges can affect the delicate structures of the inner ear, leading to sensorineural hearing loss. Routine hearing screenings following meningitis infection are recommended to detect any hearing problems early.
Vision Problems
Vision problems, such as blurred vision, double vision, or even blindness, can occur as a result of meningitis. The inflammation can affect the optic nerves and other structures of the visual system. Regular eye examinations are important to monitor and manage any vision problems.
Brain Damage
Severe cases of meningitis can cause brain damage. The inflammation in the meninges can spread to the brain tissue, leading to cognitive impairments, motor deficits, and other neurological complications. Rehabilitation and ongoing medical care are often necessary to manage and mitigate the effects of brain damage.
Memory and Cognitive Issues
Meningitis can result in memory problems and cognitive issues. Difficulties with concentration, attention, and information processing are common. Cognitive rehabilitation, memory training, and other interventions may be recommended to help individuals manage these challenges.
Seizures
Seizures can occur during meningitis, particularly in severe cases. The inflammation in the brain can trigger abnormal electrical activity and lead to seizures. Seizure management, including medication and close monitoring, is important to prevent recurrences and minimize complications.
Gait and Balance Problems
Meningitis can affect motor coordination and balance. This can result in gait abnormalities, difficulty walking, and a higher risk of falls. Physical therapy and rehabilitation programs can help improve coordination and reduce the risk of falls.
Prognosis and Recovery
The prognosis and recovery from meningitis can vary depending on several factors, including the cause of the infection, the timeliness of treatment, and the individual’s overall health. It is important to follow the healthcare provider’s recommendations and seek appropriate follow-up care.
Varies with the Cause of Meningitis
The prognosis and recovery can differ based on the cause of meningitis. Bacterial meningitis is generally more severe and associated with a higher risk of complications compared to viral and fungal meningitis. Timely diagnosis and appropriate treatment are critical in improving outcomes.
Early Detection and Treatment Improve Prognosis
Early detection and prompt treatment significantly improve the prognosis of meningitis. If meningitis is suspected, it is important to seek medical evaluation without delay. Timely initiation of appropriate treatment can prevent the spread of infection and reduce the risk of complications.
Severity and Duration of Symptoms
The severity and duration of symptoms can impact the recovery process. Some individuals may experience lingering symptoms, such as fatigue, headache, or difficulty concentrating, even after the infection has been treated. Close communication with healthcare providers and adherence to follow-up care can help manage these symptoms.
Possible Long-Term Effects
Meningitis can have long-term effects on an individual’s health and well-being. These effects can range from mild cognitive impairments or motor deficits to more significant disabilities. Rehabilitation programs and ongoing medical care are important in supporting individuals with long-term effects of meningitis.
Post-Infectious Conditions
Following an episode of meningitis, some individuals may experience post-infectious conditions, such as post-infectious encephalitis or inflammation of the brain, headaches, or psychological effects. Close monitoring and management by healthcare professionals are necessary to address these conditions and provide appropriate support.
Support and Coping Strategies
Meningitis can have a significant impact on an individual’s physical, cognitive, and emotional well-being. Various support and coping strategies are available to help individuals manage the challenges associated with meningitis.
Physical Rehabilitation
Physical rehabilitation programs, such as physiotherapy or occupational therapy, can help individuals regain strength, mobility, and coordination. These programs may include exercises, stretches, and activities tailored to the individual’s specific needs.
Speech and Language Therapy
Speech and language therapy may be necessary to address any communication or swallowing difficulties following meningitis. Therapists can provide strategies and exercises to improve speech, language, and swallowing function, as well as recommend assistive devices if needed.
Psychological Support
Meningitis can cause emotional distress, anxiety, or depression. Psychological support, such as counseling or therapy, can help individuals cope with the psychological impact of the infection. Therapists can provide strategies to manage stress, improve coping skills, and promote overall psychological well-being.
Support Groups
Engaging in support groups can provide a sense of community and understanding for individuals and their families affected by meningitis. Support groups allow individuals to connect with others who have had similar experiences, share advice, and offer emotional support.
Patient and Caregiver Education
Education is key in managing and living with meningitis. Individuals and their caregivers can benefit from learning about the infection, its potential complications, and the available treatment options. Healthcare providers can provide educational resources and information to support self-care and overall well-being.
Coping with Emotional Challenges
Coping with the emotional challenges associated with meningitis is important for recovery. Engaging in stress-reducing activities, practicing relaxation techniques, maintaining a balanced lifestyle, and seeking support from loved ones can all contribute to emotional well-being.
Conclusion
Meningitis is a serious infection that can have significant implications for an individual’s health and well-being. It is important to be aware of the causes, signs, and symptoms of meningitis, as well as the available treatment options and preventive measures. Seeking prompt medical attention, adhering to treatment plans, and accessing the appropriate support can greatly improve outcomes and enhance the quality of life for individuals affected by meningitis.