Imagine living in an area where a tiny mosquito bite has the potential to turn your life upside down. In this article, we explore the deadly impact of Dengue Hemorrhagic Fever (DHF), a viral illness transmitted by the Aedes mosquito. DHF is a silent but deadly killer that not only causes excruciating pain but can also lead to severe bleeding and organ failure. Dive into this eye-opening article to understand the dire consequences of DHF and the urgent need for prevention and treatment measures. Remember, knowledge is power when it comes to combating this relentless enemy.
Causes of Dengue Hemorrhagic Fever
Dengue Virus Transmission
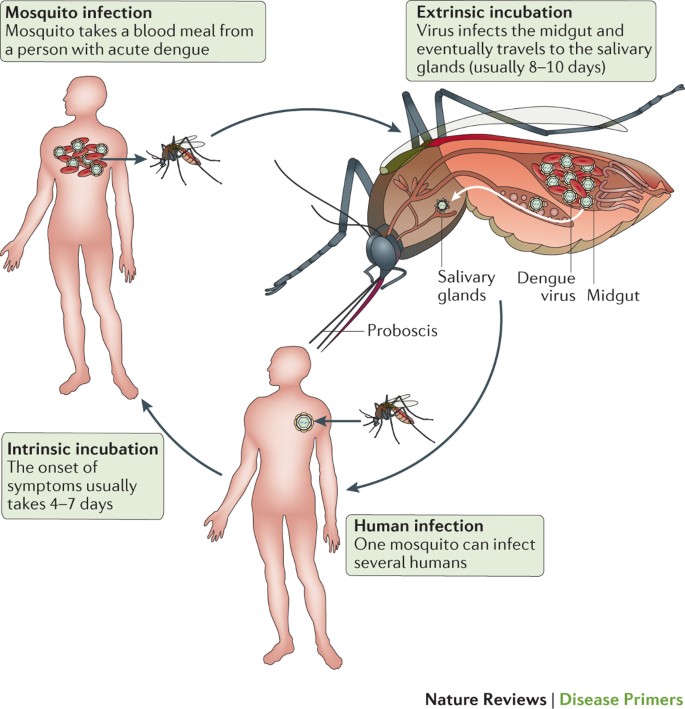
Dengue Hemorrhagic Fever (DHF) is caused by the dengue virus, which is primarily transmitted through the bite of infected female Aedes mosquitoes. These mosquitoes become carriers of the virus after biting a person infected with dengue. The virus replicates within the mosquito’s salivary glands and can be transmitted to a new host through subsequent mosquito bites. It is important to note that DHF cannot spread directly from person to person.
Mosquito Vectors
The primary mosquito species responsible for transmitting the dengue virus is Aedes aegypti. These mosquitoes are well-adapted to urban environments and are prevalent in tropical and subtropical regions around the world. Aedes mosquitoes are particularly active during the day, with peak biting activity occurring in the early morning and late afternoon. Their ability to breed in small and stagnant water bodies, such as discarded containers and flowerpots, makes them a significant public health concern.
Dengue Virus Serotypes
The dengue virus is classified into four distinct serotypes: DEN-1, DEN-2, DEN-3, and DEN-4. Each serotype represents a different variation of the virus. While infection with one serotype provides lifelong immunity against that specific serotype, subsequent infections with different serotypes can lead to more severe forms of the disease, including DHF. This phenomenon, known as antibody-dependent enhancement, occurs when the immune response from a previous infection enhances the replication of a different serotype, increasing the risk of severe complications.
Symptoms of Dengue Hemorrhagic Fever
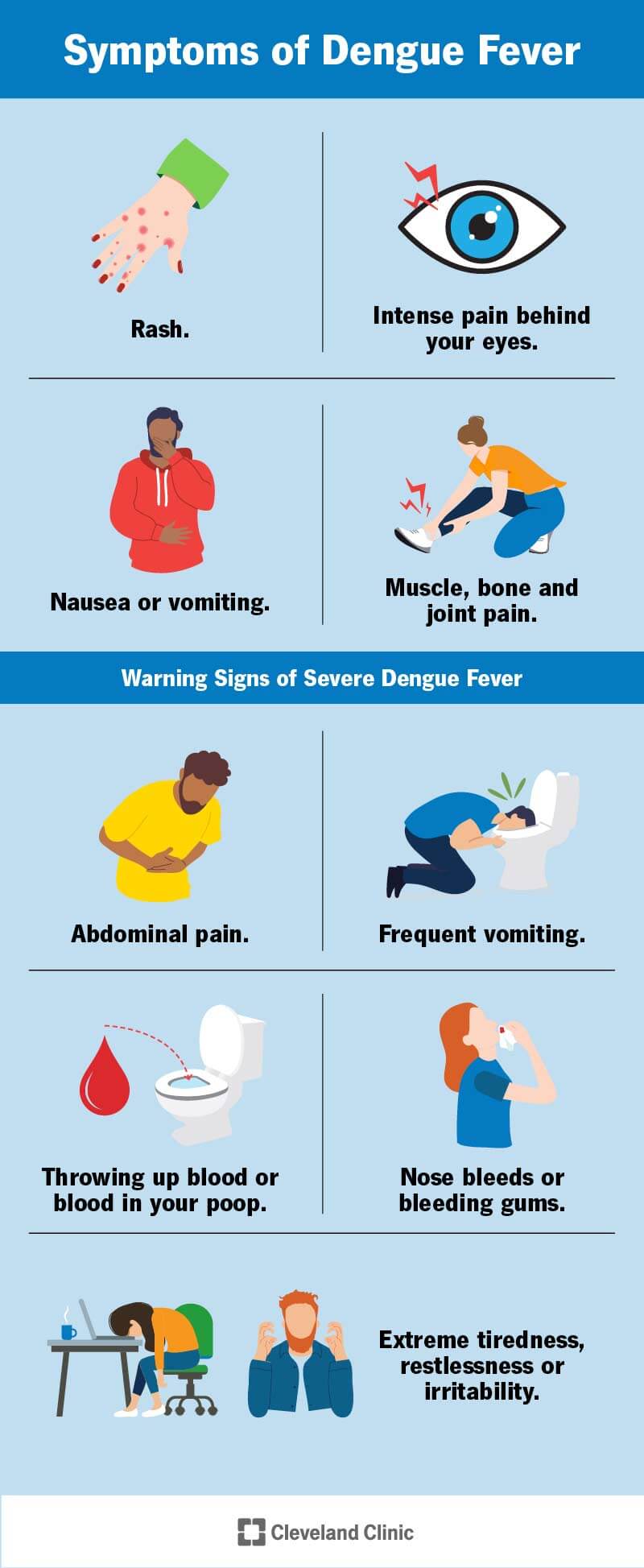
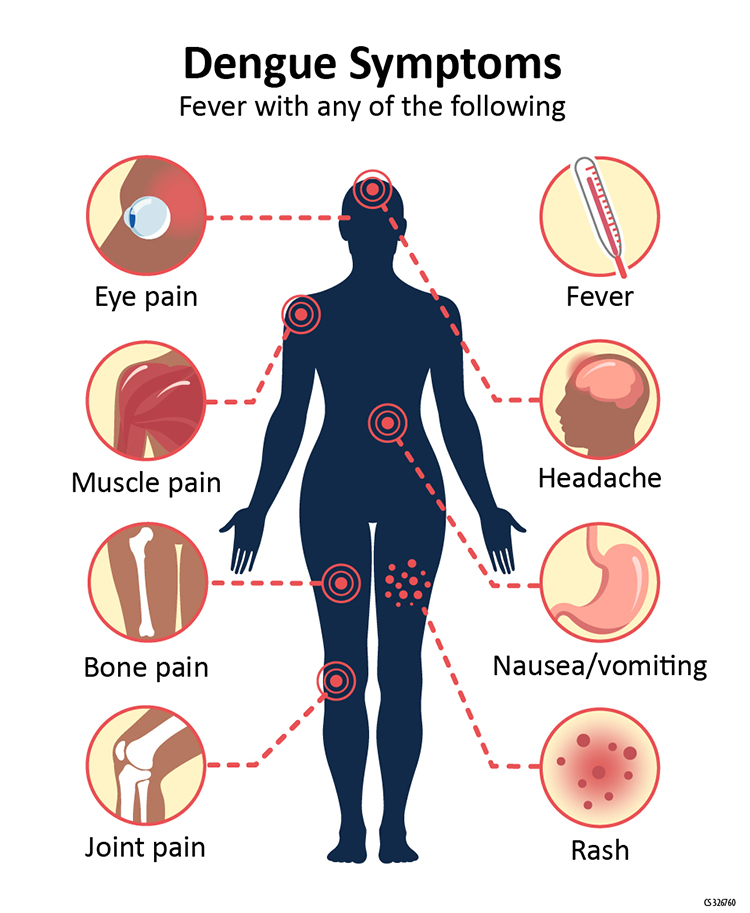
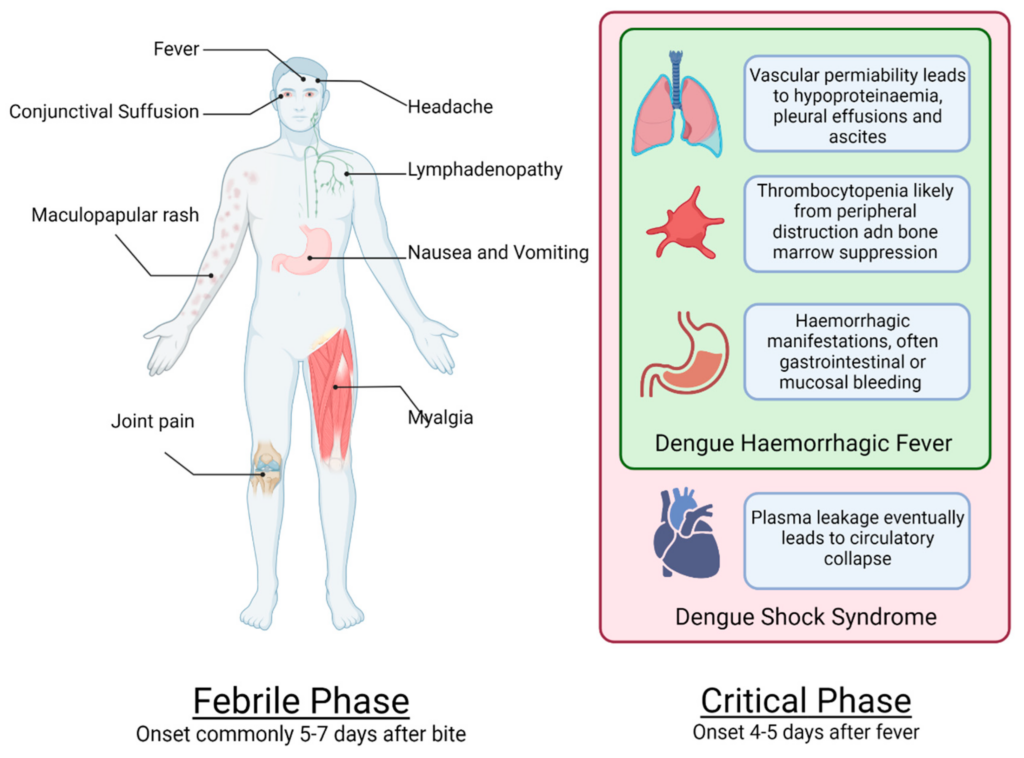
Febrile Phase
The onset of DHF is marked by a febrile phase characterized by sudden high fever, severe headaches, and joint and muscle pain. Other symptoms may include fatigue, nausea, vomiting, and a rash. The febrile phase typically lasts for 2-7 days and can mimic symptoms of other common viral illnesses, making it crucial for individuals to seek medical attention to confirm the diagnosis.
Critical Phase
Following the febrile phase, a critical phase may occur in some individuals. During this phase, the fever subsides, and there may be a brief period of improvement. However, this is often short-lived, and severe symptoms can manifest rapidly. Warning signs such as abdominal pain, persistent vomiting, bleeding from mucosal surfaces, and difficulty breathing may indicate progression to DHF. Timely medical intervention is critical during this phase to prevent further complications.
Recovery Phase
For individuals who successfully navigate the critical phase, a gradual recovery phase follows. It may take several weeks for symptoms to fully resolve, with fatigue and weakness persisting for an extended period. Adequate rest, hydration, and follow-up care are essential during this phase to ensure complete recovery.
Risk Factors for Developing Dengue Hemorrhagic Fever
Previous Dengue Infection
One of the strongest risk factors for developing DHF is a previous dengue infection. Individuals who have had a previous infection with one serotype of the virus are at higher risk of developing severe disease if subsequently infected with a different serotype. This phenomenon is thought to be due to the immune system’s response, which can inadvertently enhance the replication of the virus during a secondary infection.
Age and Sex
Age and sex can also influence the risk of developing DHF. Children under the age of 15 are more susceptible to severe forms of dengue, including DHF, compared to adults. This may be due to a combination of factors, including a weaker immune response and fewer previous dengue infections. Studies also indicate that males have a higher risk of severe disease compared to females, although the reasons for this disparity remain unclear.
Genetic Factors
Certain genetic factors may play a role in determining an individual’s susceptibility to DHF. Variations in immune system genes, such as those involved in the production and regulation of specific cytokines and chemokines, may affect the severity of the disease. Research in this area is ongoing and aims to identify genetic markers that can help predict the development of DHF and guide personalized treatment strategies.
Complications of Dengue Hemorrhagic Fever
Organ Failure
DHF can lead to various complications, including organ failure. The virus primarily affects the liver, causing impairment in its normal functioning. This can result in hepatitis and a subsequent decrease in platelet counts, leading to bleeding manifestations. In severe cases, multi-organ dysfunction syndrome (MODS) can occur, with the involvement of other vital organs such as the heart and kidneys.
Bleeding Manifestations
One of the hallmark features of DHF is bleeding manifestations, which can range from milder forms such as petechiae (tiny, pinpoint spots on the skin) and easy bruising to more severe forms such as gastrointestinal bleeding, nosebleeds, and bleeding gums. In some cases, internal bleeding may occur, leading to life-threatening situations that require immediate medical intervention.
Shock
The most severe complication of DHF is dengue shock syndrome (DSS), which is characterized by profound shock and circulatory collapse. DSS occurs due to fluid leakage from blood vessels, leading to a decrease in blood volume and subsequent inadequate perfusion of organs. Prompt and aggressive fluid resuscitation is crucial in managing DSS and preventing mortality.
Diagnosis of Dengue Hemorrhagic Fever
Clinical Evaluation
Diagnosing DHF involves a combination of clinical evaluation and laboratory tests. Healthcare providers will assess the patient’s medical history, complete a thorough physical examination, and inquire about symptoms and recent travel history to dengue-endemic areas. The presence of warning signs, such as severe abdominal pain or bleeding, helps distinguish DHF from uncomplicated dengue fever.
Laboratory Tests
Laboratory tests are essential for confirming a diagnosis of DHF. Blood samples may be collected to measure various parameters, including complete blood counts, liver function tests, and coagulation profiles. The results of these tests can indicate the presence of thrombocytopenia (low platelet count), liver involvement, and abnormal blood clotting, supporting the diagnosis of DHF.
Serological Tests
Serological tests, such as enzyme-linked immunosorbent assay (ELISA) and rapid diagnostic tests (RDTs), detect the presence of dengue-specific antibodies in the blood. These tests help determine the serotype of the virus and confirm the diagnosis of dengue infection. However, they may not be useful during the early febrile phase, as antibody levels may not have reached detectable levels.
Polymerase Chain Reaction (PCR)
In some cases, PCR tests may be used to directly detect the presence of viral genetic material in the blood or other body fluids. PCR is a highly sensitive technique that can aid in early detection, especially during the febrile phase when antibody levels are still low. PCR tests can provide rapid results and enable timely clinical management.
Prevention and Control Measures for Dengue Hemorrhagic Fever
Community Education and Awareness
Community education and awareness play a crucial role in preventing and controlling DHF. Public health initiatives should focus on educating individuals about the signs and symptoms of dengue, mosquito bite prevention strategies, and the importance of early medical consultation. By empowering communities with knowledge, they can actively participate in efforts to reduce the transmission of the virus.
Vector Control
Vector control is a fundamental component of dengue prevention and control. It involves implementing measures to reduce mosquito breeding sites and minimize human-mosquito contact. These measures may include regular removal of stagnant water sources, proper disposal of solid waste, and the use of larvicides and insecticides. Additionally, individuals can protect themselves by using mosquito repellents, wearing protective clothing, and installing window screens and bed nets.
Vaccination
In recent years, the development of dengue vaccines has provided a new tool for preventing the disease. Vaccination programs can help reduce the burden of DHF by providing immunity against dengue virus infection. However, the use of vaccines may vary across different regions, and their effectiveness depends on factors such as the circulating serotypes and the age groups targeted for vaccination. Vaccination strategies should be implemented in conjunction with other prevention and control measures for optimal impact.
Treatment of Dengue Hemorrhagic Fever
Supportive Care
Currently, there is no specific antiviral treatment for dengue. Treatment primarily focuses on supportive care to manage symptoms and prevent complications. Patients with DHF require regular monitoring of vital signs, fluid intake and output, and hematological parameters. Adequate rest, pain management, and antipyretic medications may be recommended to help alleviate symptoms and promote comfort during the febrile phase.
Fluid Replacement Therapy
Maintaining adequate fluid balance is of utmost importance in managing DHF. Intravenous fluid replacement therapy is often necessary to counteract the fluid leakage that occurs during the critical phase. The volume and type of fluids administered depend on the patient’s condition, age, and severity of symptoms. Close monitoring of fluid balance and electrolyte levels is crucial to prevent fluid overload or dehydration.
Platelet Transfusion
In cases where severe thrombocytopenia results in clinically significant bleeding, platelet transfusions may be necessary. Platelets are transfused to raise platelet counts and promote hemostasis. However, the decision to administer platelet transfusions should be based on careful evaluation of the patient’s clinical condition and the risk of bleeding complications.
Antiviral Therapy
Research is ongoing to develop specific antiviral treatments for dengue, including DHF. Several experimental antiviral drugs are being investigated, aiming to target the replication of the virus and alleviate disease severity. However, these treatments are still in the early stages of development and are not yet widely available for clinical use. Antiviral therapy remains an area of active research and holds promise for future management strategies.
Global Burden of Dengue Hemorrhagic Fever
Epidemiology
DHF is a significant global health threat, with an estimated 390 million dengue infections occurring each year. The majority of cases are reported in tropical and subtropical regions, including Southeast Asia, the Americas, and the Western Pacific. The continual increase in global travel and urbanization has contributed to its spread to previously non-endemic areas. Changing climatic conditions and the expansion of Aedes mosquito habitats further compound the global burden of DHF.
Geographical Distribution
The distribution of DHF is closely linked to the prevalence of Aedes mosquitoes. Regions with suitable climatic conditions for mosquito breeding and high population densities are at increased risk. Countries such as Brazil, India, Indonesia, Philippines, and Thailand have reported a high number of dengue cases. Efforts to control the disease must consider the unique geographical and environmental factors that contribute to its spread and focus on local context-specific interventions.
Mortality Rates
DHF can be a life-threatening condition. The case fatality rate varies, but on average, it is estimated to be around 2.5%. However, in resource-limited settings, where access to healthcare may be constrained, the mortality rates can be significantly higher. Prompt diagnosis, early medical intervention, and adequate supportive care are essential in reducing mortality rates associated with DHF.

Public Health Initiatives and Strategies to Combat Dengue Hemorrhagic Fever
Integrated Vector Management
Integrated vector management (IVM) is a comprehensive approach that combines various methods to control mosquito populations. IVM strategies include surveillance, source reduction, larviciding, insecticide spraying, and community engagement. By implementing IVM, public health authorities can effectively target different stages of the mosquito lifecycle and disrupt the transmission of the dengue virus.
Surveillance Systems
Establishing robust surveillance systems is crucial for monitoring the epidemiology and patterns of dengue transmission. Timely detection, reporting, and investigation of cases enable public health authorities to implement targeted control measures. Efficient surveillance systems enable the identification of high-risk areas, early warning of outbreaks, and evaluation of the impact of prevention and control strategies.
Health Promotion Campaigns
Health promotion campaigns serve as a vital tool in raising community awareness about DHF and promoting preventive behaviors. These campaigns can utilize various communication channels, including traditional media, social media, and community engagement activities. By disseminating accurate and timely information, health promotion campaigns empower individuals to protect themselves and their communities from dengue.
Challenges in Controlling Dengue Hemorrhagic Fever
Increased Urbanization
The rapid growth of urban areas poses significant challenges in controlling DHF. Factors such as unplanned urbanization, inadequate public infrastructure, and inadequate waste management contribute to the proliferation of Aedes mosquito breeding sites. Overcrowded living conditions, limited access to healthcare facilities, and poor urban planning further exacerbate the risk of dengue transmission. Addressing these challenges requires a multi-sectoral approach, involving urban planners, public health authorities, and community engagement.
Climate Change
Climate change has a direct impact on the distribution and transmission dynamics of dengue. Rising temperatures and altered rainfall patterns create favorable conditions for mosquito breeding and survival. Additionally, extreme weather events such as floods and hurricanes can disrupt control programs and lead to increased transmission. Adapting to the changing climate necessitates the implementation of resilient strategies that account for the anticipated challenges posed by climate change.
Limited Resources
Limited resources, particularly in resource-limited settings, pose significant barriers to effective DHF control. Inadequate funding, personnel, and infrastructure hinder the implementation of prevention and control measures. Additionally, access to diagnostic and treatment facilities may be limited, leaving communities vulnerable to the severe consequences of DHF. International collaborations, capacity building initiatives, and sustainable financing models are essential in addressing these resource constraints and strengthening health systems.