You may not realize it, but there is a whole world of people out there who struggle with a condition called Celiac Disease. This fascinating article aims to shed light on the ins and outs of this often misunderstood condition, explaining what it is, how it affects the body, and the importance of a gluten-free diet for those living with Celiac Disease. So, buckle up and get ready to embark on a journey of knowledge and understanding, discovering the hidden truths of Celiac Disease.
Definition
What is celiac disease?
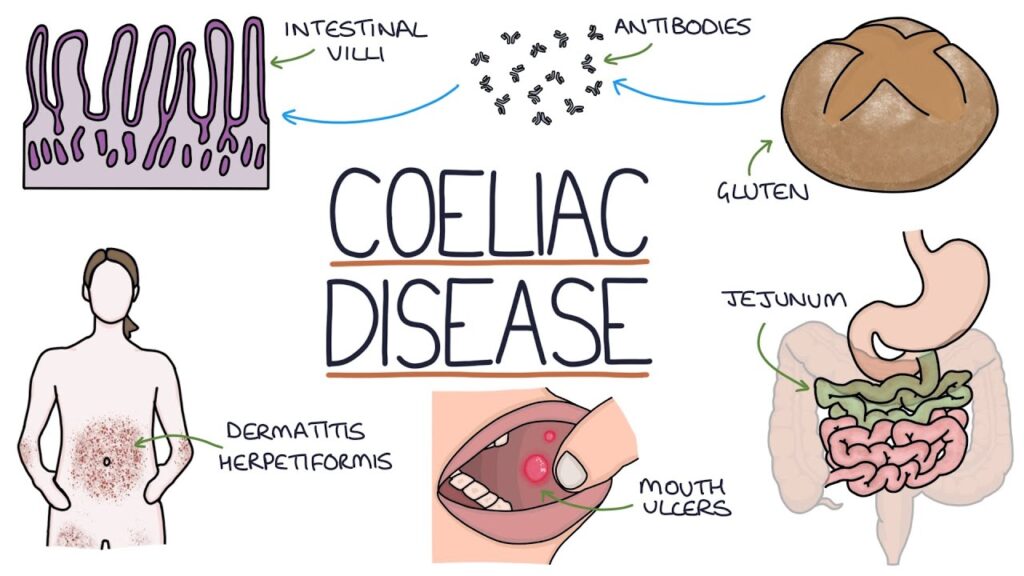
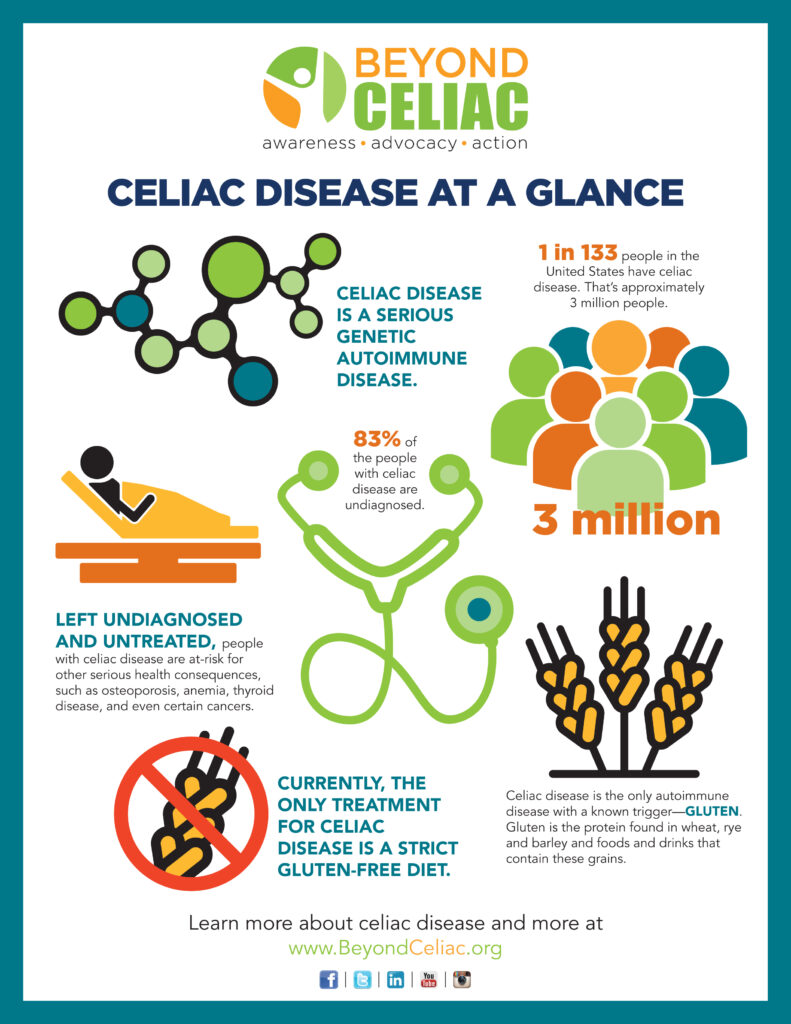
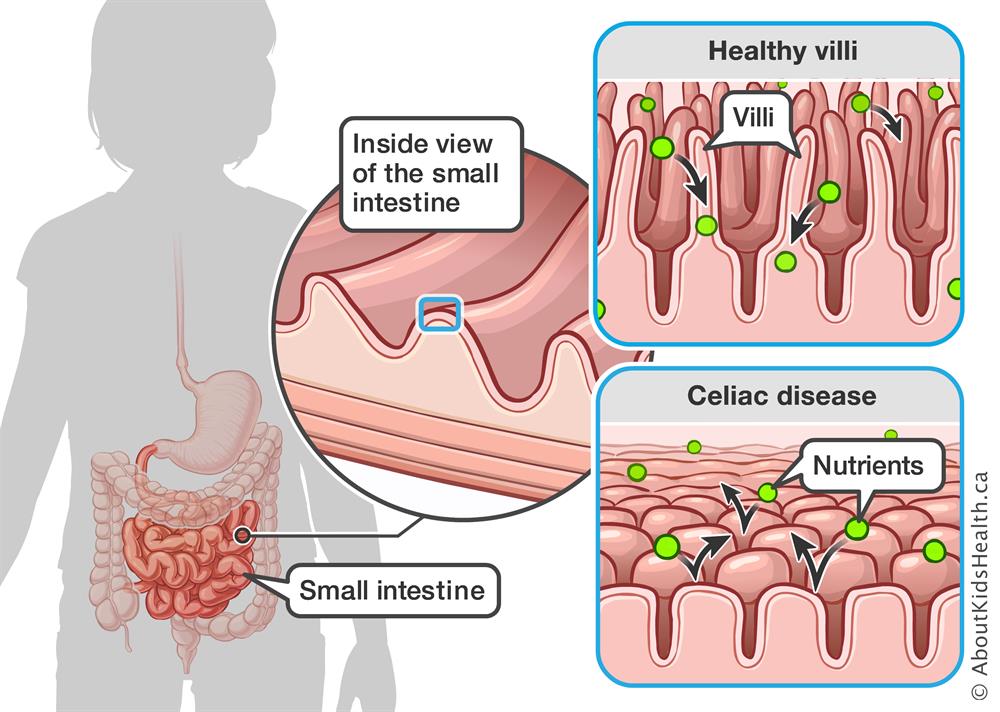
Celiac disease is an autoimmune disorder that affects the small intestine and is triggered by the ingestion of gluten. Gluten is a protein found in wheat, barley, and rye. When a person with celiac disease consumes gluten, their immune system mistakenly attacks the small intestine, causing inflammation and damage to the lining of the intestine. This chronic condition can lead to various symptoms and complications if left untreated.
Causes of celiac disease
The exact cause of celiac disease is not yet fully understood. However, research suggests that a combination of genetic and environmental factors play a role in its development. Certain genes, such as the human leukocyte antigen (HLA) genes, seem to increase the risk of developing the disease. Additionally, factors such as a family history of celiac disease, the timing of gluten introduction in an infant’s diet, and certain environmental triggers may contribute to its onset.
Symptoms
Digestive symptoms
Digestive symptoms are common in individuals with celiac disease. These symptoms may include abdominal pain, bloating, diarrhea, constipation, and vomiting. The inflammation and damage to the small intestine disrupt the normal absorption of nutrients, leading to digestive issues. It is important to note that not all individuals with celiac disease experience digestive symptoms.
Non-digestive symptoms
Celiac disease can also manifest with non-digestive symptoms, making it challenging to diagnose. Some of these symptoms may include fatigue, anemia, bone and joint pain, skin rash (dermatitis herpetiformis), headaches, and depression. These symptoms can vary widely among individuals and may be mistaken for other conditions, leading to delayed diagnosis.
Diagnosis
Blood tests
The first step in diagnosing celiac disease is usually a blood test. This test measures the levels of certain antibodies that are typically elevated in individuals with the disease. The most common blood test for celiac disease is the tissue transglutaminase antibody (tTG-IgA) test. If the blood test results suggest celiac disease, further testing is typically done to confirm the diagnosis.
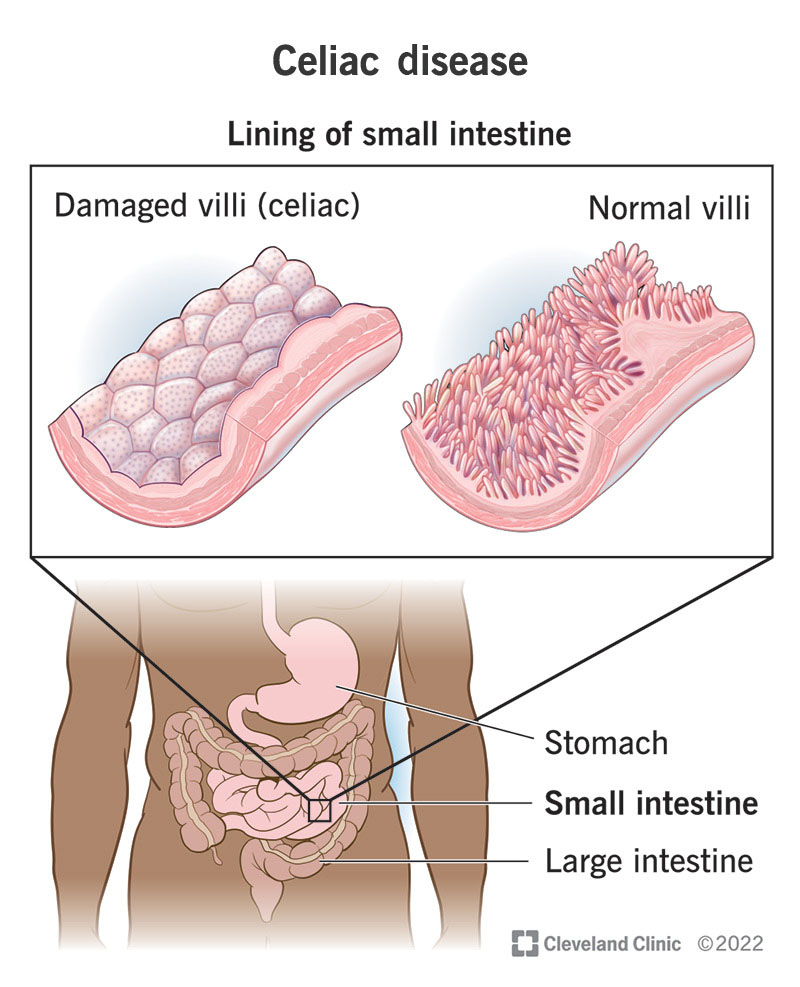
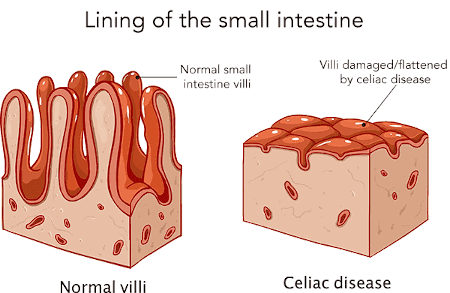
Biopsy
A biopsy of the small intestine is considered the gold standard for diagnosing celiac disease. During a biopsy, a small sample of tissue is taken from the small intestine and examined for damage to the intestinal lining. This procedure is usually done using an endoscope inserted through the mouth or nose. A biopsy can confirm the presence of celiac disease and assess the extent of intestinal damage.
Genetic testing
Genetic testing can be used to determine if a person has the specific genes associated with celiac disease. However, it should be noted that having these genes does not necessarily mean a person will develop the disease. Genetic testing can be helpful in certain situations, such as when a person is already on a gluten-free diet or when the results of other tests are inconclusive.
Treatment
Gluten-free diet
The primary treatment for celiac disease is a strict lifelong gluten-free diet. This means avoiding all sources of gluten, including wheat, barley, rye, and products derived from these grains. Following a gluten-free diet allows the small intestine to heal and prevents further damage. It is important to work closely with a healthcare professional and a registered dietitian to ensure adequate nutrition while on a gluten-free diet.
Supplements
In some cases, individuals with celiac disease may need to take supplements to address nutritional deficiencies. Common deficiencies in celiac disease include iron, vitamin D, calcium, and B vitamins. Supplements may be prescribed to help restore and maintain optimal nutrient levels.
Medications
There are currently no medications available to treat celiac disease itself. However, medications may be prescribed to manage certain symptoms or complications associated with the disease. For example, medications may be used to address digestive symptoms, such as acid reflux or irritable bowel syndrome, that may coexist with celiac disease.
Complications
Malabsorption
One of the main complications of untreated celiac disease is malabsorption. The damage to the small intestine impairs its ability to absorb nutrients properly. As a result, individuals with celiac disease may experience nutrient deficiencies and have difficulty maintaining a healthy weight. Malabsorption can lead to a wide range of health problems if not adequately addressed.
Nutritional deficiencies
Celiac disease can cause various nutritional deficiencies due to the malabsorption of nutrients. Common deficiencies include iron, calcium, vitamin D, vitamin B12, and folate. These deficiencies can have long-term effects on overall health, leading to conditions such as anemia, osteoporosis, and neurologic disorders if left untreated.
Osteoporosis
Untreated celiac disease can also increase the risk of developing osteoporosis, a condition characterized by weak and brittle bones. Chronic inflammation and malabsorption of calcium and vitamin D contribute to the loss of bone density. It is essential for individuals with celiac disease to maintain adequate calcium and vitamin D levels, in addition to following a gluten-free diet, to minimize the risk of osteoporosis.
Management
Dietary management
Managing celiac disease involves strict adherence to a gluten-free diet. This means avoiding all sources of gluten and being diligent in reading food labels to identify hidden sources of gluten. It is crucial to educate oneself about safe and gluten-free food options and to communicate with food establishments about dietary requirements when dining out.
Reading food labels
When living with celiac disease, reading food labels becomes a necessary habit. Food labels can provide information about the presence of gluten or potential cross-contamination. Key terms to look out for include wheat, barley, rye, malt, and modified food starch. Familiarizing oneself with these terms and understanding cross-contamination risks can help make informed food choices.
Cross-contamination prevention
Preventing cross-contamination is an important aspect of managing celiac disease. Cross-contamination occurs when gluten-containing and gluten-free ingredients come into contact with each other. This can happen during food preparation, storage, or cooking. To prevent cross-contamination, it is essential to use separate cooking utensils, cutting boards, and to clean surfaces thoroughly. Additionally, individuals with celiac disease should be cautious when eating out or using shared kitchen facilities.
Influence on Daily Life
Challenges faced
Living with celiac disease can present several challenges. Following a strict gluten-free diet requires careful planning, label reading, and meal preparation. Finding gluten-free options while dining out or attending social events can be a challenge, and individuals with celiac disease may feel limited in their food choices. Adapting to the necessary lifestyle changes and establishing a support network can help overcome these challenges.
Social implications
Celiac disease can have social implications, especially when it comes to dining out or attending social gatherings. It can be difficult to explain the dietary restrictions and ensure that meals are prepared safely. People with celiac disease may feel excluded or misunderstood by others who are not familiar with the condition. Building awareness and open communication with friends, family, and social circles can help create a supportive environment.
Traveling and dining out
Traveling and dining out can become more complicated for individuals with celiac disease. Different countries and cultures may have varying levels of awareness and understanding about celiac disease and gluten-free options. Researching and planning ahead, communicating dietary needs to airline and hotel staff, and being prepared with gluten-free snacks can help make traveling and dining out more manageable.
Alternative and Gluten-Free Diets
Paleo diet
The paleo diet has gained popularity, especially among individuals with celiac disease and gluten sensitivity. The paleo diet focuses on consuming whole, unprocessed foods and excludes grains, including gluten-containing grains. Some individuals with celiac disease find relief of symptoms and improved overall health by following a paleo diet. However, it is important to ensure that nutrient needs are met and to work with a healthcare professional or dietitian to ensure a balanced diet.
Low FODMAP diet
The low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet is often recommended for individuals with irritable bowel syndrome (IBS). It involves restricting certain types of carbohydrates that can be poorly absorbed in the small intestine and may cause digestive symptoms. While the low FODMAP diet is not specifically designed for celiac disease, some individuals with celiac disease may find it helpful in managing their symptoms.
Risks of Gluten-Free Diet
Lack of nutrients
Following a gluten-free diet may increase the risk of certain nutrient deficiencies if not properly balanced. Gluten-containing grains, such as wheat, are a common source of dietary fiber, B vitamins, and iron. It is important for individuals on a gluten-free diet to ensure an adequate intake of these nutrients through alternative food sources or appropriate supplementation.
Higher costs
Gluten-free products are often more expensive than their gluten-containing counterparts. The production and manufacturing processes involved in gluten-free products can drive up their cost. Additionally, individuals with celiac disease may need to be cautious about cross-contamination risks, leading to more expensive food choices and dining out options. The financial burden of a gluten-free diet should be considered and managed accordingly.
Emerging Research and Current Trends
Non-gluten triggers
While gluten is the primary trigger for celiac disease, some individuals may experience symptoms even when following a strict gluten-free diet. Emerging research suggests that other components of wheat, such as amylase-trypsin inhibitors (ATIs), may contribute to symptoms in some individuals. Further research is needed to better understand these non-gluten triggers and their effects on people with celiac disease.
Potential new treatments
Researchers are actively exploring potential new treatments for celiac disease. One approach being investigated is the development of enzyme therapies that can break down gluten in the digestive system, reducing the harmful effects on the small intestine. Other strategies include the use of medications to modulate the immune response in individuals with celiac disease. While these potential treatments are promising, they are still in the experimental stages and further research is needed.
Celiac disease awareness
There is a growing awareness of celiac disease in recent years, leading to improved diagnosis rates and increased availability of gluten-free products and options. Organizations and support groups dedicated to celiac disease awareness have been instrumental in providing resources, education, and support to individuals with celiac disease and their families. Continued efforts to raise awareness, promote research, and improve access to gluten-free options are essential in supporting those affected by celiac disease.
In conclusion, celiac disease is a chronic autoimmune disorder that requires lifelong management through a strict gluten-free diet. Recognizing the symptoms, obtaining a proper diagnosis, and understanding the dietary and lifestyle adjustments necessary are key to effectively managing the condition. With increased awareness, support, and ongoing research, individuals with celiac disease can lead fulfilling lives while prioritizing their health and well-being.